Interscalene_Brachial_Plexus_Block_Info
advertisement

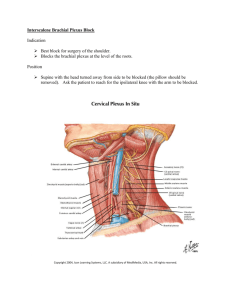
Interscalene Brachial Plexus Block Scott Pearson & Eric Petrunak (Original Authors: Brown, Novak, Underwood, 2003) Diagram obtained from Brown, Novak, & Underwood 2003 Anesthesia Class Project PowerPoint on Interscalene Plexus Block. Indications The interscalene approach is used for surgical procedures of the shoulder or upper arm and blocks brachial plexus nerves. The interscalene block is useful for post-operative pain control and is commonly utilized in conjunction with general anesthesia but can be used alone. The interscalene approach to brachial plexus block is most intense in the C5-C7 dermatomes and least intense in the C8-T1 dermatomes, therefore surgical anesthesia is not optimal for areas of ulnar innervation. This block can also be used for pain management of shoulder arthrosis, arthritis, and complex regional pain syndromes. Drugs Bupivacaine 0.25% or 0.5% is frequently used. The 0.25% has an onset of 20-30 minutes and duration of 7-15 hours. The 0.5% has an onset of 10-20 minutes and duration of 9-20 hours. Epinephrine does not prolong the duration of Bupivacaine. 0.1cc of sodium bicarbonate per 10cc of local can hasten the onset time. Bupivacaine is frequently used since it has a long duration to provide post-op analgesia. Other drugs that can be used include: Procaine 2%, Chlorprocaine 2%, Lidocaine 1%, Mepivacaine 1%, and Prilocaine 1%. These other drugs are less frequently used as they have much shorter duration of actions, even with Epinephrine, therefore are less optimal for post-op pain control. 20-40 cc of local anesthetic is used depending on extent of block required, patient condition, and the stature of the patient. Anatomy The brachial plexus includes spinal nerves C5-T1. The brachial plexus may contain C4 and T2 as well. Cervical spinal nerves blend into trunks between the anterior and middle scalene muscles. Brachial plexus cervical nerves pass laterally in a deep groove in the superior surface of the cervical vertebrae transverse process. This groove separates the transverse process into anterior and posterior tubercles. These tubercles are the origin of the anterior and medial scalene muscles. In a normal person the C6 transverse process is superficial and no more than 1.5-2 cm beneath the skin. The scalene muscles pass under the midpoint of the clavicle and insert on the 1st rib. The subclavian artery runs between the anterior and middle scalene muscles. Refer to the anatomy website for further shoulder and brachial plexus anatomy. http://www.pitt.edu/~anat/Extremities/Shoulder/Shoulder.htm Technique The patient is supine with the head flexed, not rotated, to the contralateral side. A towel is placed under the head and the patient is asked to hold the ipsilateral shoulder down as though reaching for the knee. The external jugular often crosses the interscalene groove at the level of the cricoid cartilage. The SCM is palpated first. With the patient raising his head in a sniffing position the scalene muscle stiffens. The interscalene groove between the anterior and medial scalene is found by rolling the fingers off the lateral edge of the SCM. The groove can be felt at the peak of deep inspiration as the scalenes are accessory muscles of ventilation. The groove is palpated as high as possible. The patient can then relax and the level at the cricoid is marked. The transverse process of C6 can usually be palpated and is directly opposite to the entry point. The site is cleaned and prepped with a povidone-iodine solution 2 inches in circumference to the injection site. A skin wheal is performed with plain 0.5% Lidocaine. A 22G 1.5inch B bevel needle is introduced perpendicular to the skin (not perpendicular to the spinal axis) until a distinct pop is felt indicating penetration of the fascia. The needle is advanced in medial and caudal directions until a parethesia or evoked muscle contraction in the arm is elicited. Evoked muscle contraction can be accomplished by attaching the negative cathode of a PNS to the needle with an alligator clip. The positive cathode is attached to an EKG electrode on the chest. Set the PNS to 5-10 mA and advance the needle until cyclic muscle contraction at or distal to the shoulder is noted. Reduce the current to 0.5-1 mA and slowly advance/withdraw the needle until maximum contractions are noted. Aspiration is performed first to check for intravascular penetration then local is injected in small increments to detect intraneural or intraarterial injection. If bone is encountered without elicitation of parethesias or motor response stimulation then needle advancement was likely to be too anterior and the needle is redirected. 2-3cc of local is injected 1st and motor activity fade is observed in 10-15 seconds. Aspiration should be done every 5cc of injection. After injection the syringe is removed and retrograde flow of local should be observed for, as this is indicative of proper local anesthetic placement. Proximal pressure can be applied to favor spread of local distally. 20-40 cc of local anesthetic is used depending on extent of block required, patient condition, and the stature of the patient. 40cc of local does not guarantee spread to cover ulnar nervation. Photo obtained from Brown, Novak, & Underwood 2003 Anesthesia Class Project PowerPoint on Interscalene Plexus Block. Photo obtained from Brown, Novak, & Underwood 2003 Anesthesia Class Project PowerPoint on Interscalene Plexus Block. Block Assessment Successful neuraxial blockade relies upon spread of the local anesthetic, therefore adequate “soak time” of 20-30 minutes after block administration should be allowed to achieve adequate surgical anesthesia. Care must be taken when assessing block as injuries to the arm or body can occur if the arm is not supported and allowed to fall onto the patient or down to their side. Motor blockade occurs before sensory block. Motor and sensory block will occur proximally in the shoulder 1st and spreads distally. Axillary nerve motor block can be assessed by asking the patient to abduct his upper arm against resistance. Axillary nerve sensory block can be assessed by checking for anesthesia of the lateral aspect of the upper arm. Musculocutaneous nerve motor block is assessed by asking the patient to flex at the elbow. Musculocutaneous nerve sensory block is assessed by checking for anesthesia of the medial aspect of the forearm. Radial nerve motor block can be assessed by asking the patient to extend the forearm against resistance. Radial nerve sensory block can be assessed by checking for anesthesia of the webspace between the thumb and first finger. Median nerve motor block can be assessed by asking the patient to make a fist while holding extension pressure on the 1st and 2nd fingers. Median nerve sensory block can be assessed by checking for anesthesia of the palmar surface of the thumb and 1st two and half fingers. Ulnar nerve blockade is frequently missed by this block. Ulnar nerve motor block can be assessed by asking the patient to abduct his “pinky” finger against pressure. Ulnar nerve sensory block can be assessed by checking for anesthesia of the ring and “pinky” fingers. Complications Complications can occur due to the proximity of other anatomical structures. Blockade of the stellate ganglion can occur with resultant Horner’s syndrome (triad of myosis, ptosis, and anhidrosis). The phrenic nerve can be blocked with resultant dyspnea. This block is not done bilaterally to avoid accidentally bilateral blockade of the phrenic nerves. The recurrent laryngeal nerve can be blocked with resultant hoarseness. Accidental injection into the vertebral artery can lead to rapid seizures and CNS toxicity. Accidental injection into the cervical epidural, subarachnoid, or subdural space can lead to epidural anesthesia or a high spinal. Advancement of the needle to far lateral can result in pneumothorax. Hematoma can occur from accidental puncture of the vertebral or subclavian artery or the subclavian vein. Direct nerve injury can occur due to needle trauma. It should be noted that most complications can be avoided by remaining “superficial”. 1-1.5 cm should be adequate to reach the brachial plexus and illicit a parasthesia. References 1. Barash, Cullen, Stoelting. Clinical Anesthesia. 4th ed. Baltimore. Lippincott Williams & Williams. 2001. 2. Brown, Novak, Underwood. Interscalene Plexus Block. 2003 Anesthesia Class Project. 3. Cousins, Bridenbaugh. Neural Blockade. 3rd ed. Philadelphia. Lippincott – Raven. 1998. 4. Morgan, Mikhail, Murray. Clinical Anesthesiology. 3rd ed. New York. Lange. 2002. 5. Reese. Upper Extremity Blocks. AANA. Study Questions 1. What nerves come from the brachial plexus? 2. What are some complications of an Interscalene block? Study Questions 1. What nerves come from the brachial plexus? Axillary, Musculocutaneous, Radial, Median, & Ulnar nerves 2. What are some complications of an Interscalene block? Dyspnea from pneumothorax or phrenic nerve blockade Seizures or CNS toxicity from intravascular injection Horner’s syndrome from stellate ganglion blockade Hoarseness from recurrent laryngeal nerve blockade High spinal from subarachnoid/subdural injection Hematoma Nerve injury from needle trauma