Radial nerve entrapment
advertisement

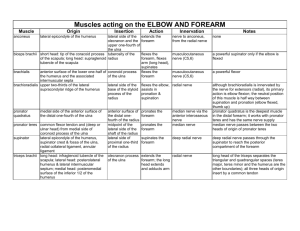
RADIAL NERVE ENTRAPMENT Anatomy Terminal branch of posterior cord (C5-C7) Lies behind axillary artery Travels thru lateral triangular space with profunda brachii artery o Lateral – humerus o Superior – teres major o Medial – long head of triceps Lies deep to the lateral head and superficial to the medial head near the spiral groove Pierces the lateral intermuscular septum 10cm above the lateral epicondyle with the radial collateral artery in a groove between brachialis and brachioradialis and distally between brachialis and ECRL Branches o Posterior cutaneous nerve of arm o Triceps motor branches (4 branches - long, medial, lateral, medial) before spiral groove o Inferior lateral cutaneous nerve of arm o Posterior cutaneous nerve of forearm o Brachialis motor (1-3 branches) 3-9cm above epicondylar line o Brachioradialis (1-3 branches) 3-6cm above epicondylar line. May also arise from SRN o ECRL (1-3 branches) 6cm above to 2.5cm below epicondyles or from PIN o anconeus Emerges anterior to lateral epicondyle o Superficial branch courses under brachioradialis, and emerges between BR and ECRL 7cm proximal to wrist o Deep branch gives off ECRB (rarely from main trunk or SRN) passes through superficial and deep heads of supinator gives supinator 2-5 branches Exits supinator and divides into deep and superficial parts Superficial supplies ECU (1.3cm), EDC (1.5cm) and EDM (1.8cm) Deep supplies APL(5.6cm), EPB(6.5cm), EIP(6.8cm) and EPL(7.5cm) High radial nerve compression 1. Anomalous muscle o accessory scapularis-teres-latissimus muscle – lateral margin of scapula fusing with insertion of subscapularis 2. mid-humeral fracture o may be acute or occur late (associated with healing callus) 3. Lateral intermuscular septum 4. compression at the fibrous arch of the lateral head of the triceps muscle Operative Management Anterolateral approach Lateral decubitus with upper limb free draped, no torniquet Incision from between deltoid and lateral triceps to between biceps and brachioradialis Track radial nerve distal to proximal, between long/lateral triceps dividing tendons of teres major and lat dorsi. Mangement of nerve injury in closed humeral fractures Incidence: 1.8 to 16% of humeral fractures occurs most commonly with middle third humeral fractures & in Holstein Lewis fractures (distal 1/3rd) Controversial management, 3 main methods 1. Early exploration o Case for: Status of nerve can be ascertained Stabilisation of fracture by internal fixation Early operation is easier and safer o Case against Most studies indicate that majority of closed fractures will not have nerve entrapment or laceration even in high velocity injuries o Main indications Open fracture - nerve lacerations most frequently occur in open fractures associated with high energies with significant crush/avulsion. Unable to reduce closed Associated vascular injury Patients with multiple trauma o Palsy after closed reduction is not a absolute indication for immediate exploration 2. Nerve exploration at 6-8 weeks if no return 3. Nerve exploration >3months o Well documented that initial signs of recovery may not appear until 45 months after o Advantage: Avoids unnecessary operation in most patients Most will achieve full recovery Humerus fracture will be healed o Radial nerve can be repaired successfully 9-16 months after injury Radial nerve paralysis associated with fractures of the humerus. A review of 62 cases. Shah Clin Orthop Relat Res. 1983 o Conservative management led to excellent nerve recovery in all groups of patients. o Overall, 95% of the patients with radial nerve paralysis recovered normal or near normal function. o All patients with secondary paralysis had full functional recovery of the radial nerve. Holstein Lewis fracture Posterior Interosseous Nerve Syndrome Clinical Typically insidious Weakness of finger extension, radial drift with wrist extension May be complete or incomplete May be confused with EDC rupture in rheumatoid patients o RA patients are also more prone to getting PINS from synovitis o First fibres to be affected are EDC to RF and LF o May present with isolated EPL paralysis o Use tenodesis effect and EMG to rule out diagnosis Sites of compression 1. lateral intermuscular septum 2. thickened fascial tissues superficial to radiocapitellar joint 3. leash of vessels from radial recurrent artery (leash of Henry) 4. fibrous edge of ECRB 5. proximal edge of supinator (arcade of Frohse) – fibrous arch from lateral epicondyle 6. distal edge of supinator Investigations xray to rule out unreduced radial head and humeral fractures U/S useful to screen for ganglia MRI also good for soft tissue tumors Electrodiagnostics Management Nonoperative For idiopathic or post traction injuries Rest, splint, analgesics Corticosteroid injections in RA patients (radiocapitellar joint) Failure to improve after 4-12 weeks of conservative management should proceeed to surgery Operative Anterior approach (Henry) Approach on medial border of brachioradialis longitudinal incision at point just lateral & proximal to biceps tendon (at the flexor crease of the elbow) extend it distally in forearm along medial border of brachioradialis towards the radial styloid BR is retracted laterally and the pronator teres is retracted medially; Advantage: good view of nerve proximal to it entering into forearm Disadvantage: bad view of nerve distal end of supinator Posterior approach (Thompson) Incision in line from middle of dorsal wrist to lateral epicondyle along dorsal border of mobile wad of Henry(BR,ERCL,ERCB) Approach in between EDC and ECRB much less soft tissue stripping is required as compared to anterior approach Advantage: good view of the PIN throughout supinator especially distal end Disadvantage: bad view of nerve proximal to supinator Transmucular brachioradialis split BR muscle belly split bluntly towards the radial head Advantage: good view at arcade of Frohse Best approach for radial tunnel syndrome BR-ERCL approach Approach between lateral border of BR and ECRL Best done in combination with EDC-ECRB split Radial Tunnel Syndrome Boundaries 1. Medial: biceps tendon 2. Floor: radiocapitellar joint 3. Lateral: mobile wad BR, ECRL, ECRB 4. Roof: BR 5. Distal: arcade of Frohse Clinical often appears in individuals whose work requires repetitive elbow extension or forearm rotation. Pain syndrome with weakness due to pain Symptoms are intensified by extending the elbow and pronating the forearm Typically deep and aching pain on the lateral aspect of elbow Tenderness over the anterior head of radius(feel over the volar border of the mobile wad of Henry May be worse at night Main differential is lateral epicondylitis but tenderness of RTS is more distal Provocation tests a. Middle finger test – resisted middle finger extension, push on dorsum of proximal phalanx of middle finger. Positive if patient gets pain over ECRB b. Resisted supination in full elbow extension Electrodiagnostic studies may not be helpful Management Nonoperative Should be tried in most instances and surgery reserved for failure Splint in supination and wrist extension Superficial Radial Nerve Compression Syndrome (Wartenberg syndrome) Clinical pain over the distal radial forearm associated with paresthesias over the dorsal radial hand. Worse with wrist movement or when tightly pinching the thumb and index digit. positive Tinel sign over the SRN and local tenderness. Hyperpronation of the forearm can cause a positive Tinel sign. Differentiate from De Quervains stenosing tenovaginitis may be difficult – 96% of patients will have positive Finklestein’s test o Injecting local anaesthetic into the proximal part of SRN under BR o Tinels sign o electrodiagnostics Site of compression Usual site of compression is where SRN goes through fascia between BR and ECRL May occur with nerve entrapment in scar following recent accident Management Nonoperative measures is tried before surgery Operative 5cm incision over distal 1/3rd radius in line with radial styloid to lateral epicondyle