Anesthetic Implications of Wolff-Parkinson
advertisement
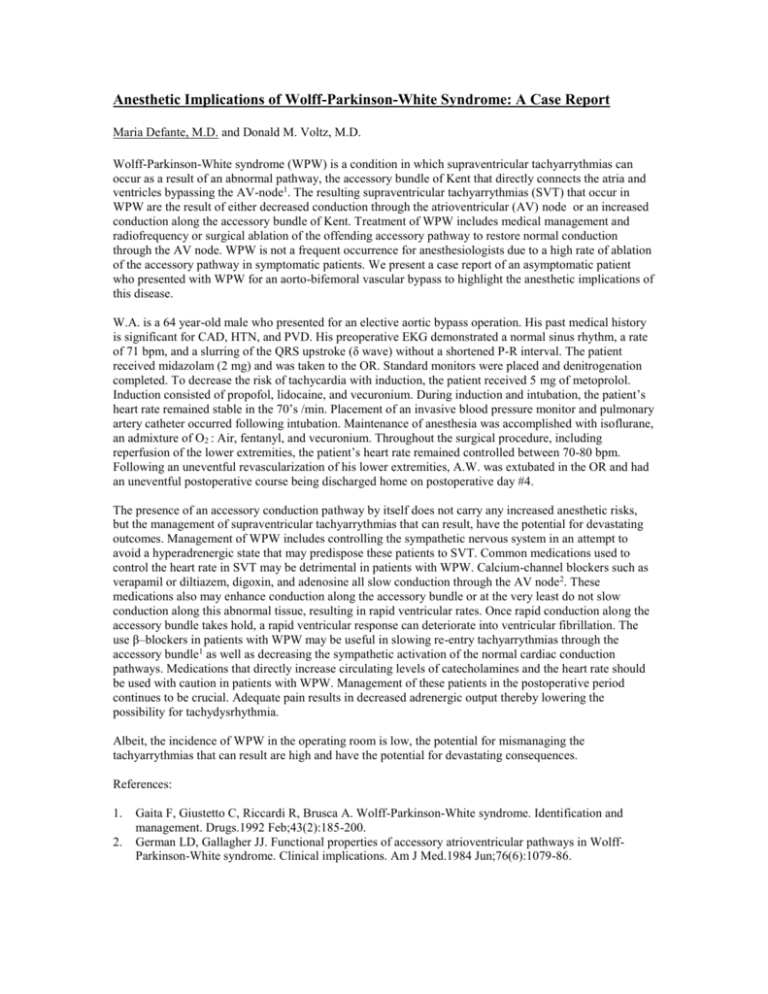
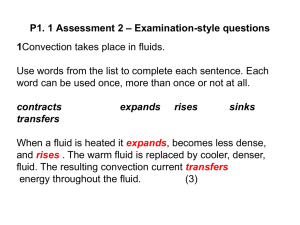
Anesthetic Implications of Wolff-Parkinson-White Syndrome: A Case Report Maria Defante, M.D. and Donald M. Voltz, M.D. Wolff-Parkinson-White syndrome (WPW) is a condition in which supraventricular tachyarrythmias can occur as a result of an abnormal pathway, the accessory bundle of Kent that directly connects the atria and ventricles bypassing the AV-node1. The resulting supraventricular tachyarrythmias (SVT) that occur in WPW are the result of either decreased conduction through the atrioventricular (AV) node or an increased conduction along the accessory bundle of Kent. Treatment of WPW includes medical management and radiofrequency or surgical ablation of the offending accessory pathway to restore normal conduction through the AV node. WPW is not a frequent occurrence for anesthesiologists due to a high rate of ablation of the accessory pathway in symptomatic patients. We present a case report of an asymptomatic patient who presented with WPW for an aorto-bifemoral vascular bypass to highlight the anesthetic implications of this disease. W.A. is a 64 year-old male who presented for an elective aortic bypass operation. His past medical history is significant for CAD, HTN, and PVD. His preoperative EKG demonstrated a normal sinus rhythm, a rate of 71 bpm, and a slurring of the QRS upstroke (δ wave) without a shortened P-R interval. The patient received midazolam (2 mg) and was taken to the OR. Standard monitors were placed and denitrogenation completed. To decrease the risk of tachycardia with induction, the patient received 5 mg of metoprolol. Induction consisted of propofol, lidocaine, and vecuronium. During induction and intubation, the patient’s heart rate remained stable in the 70’s /min. Placement of an invasive blood pressure monitor and pulmonary artery catheter occurred following intubation. Maintenance of anesthesia was accomplished with isoflurane, an admixture of O2 : Air, fentanyl, and vecuronium. Throughout the surgical procedure, including reperfusion of the lower extremities, the patient’s heart rate remained controlled between 70-80 bpm. Following an uneventful revascularization of his lower extremities, A.W. was extubated in the OR and had an uneventful postoperative course being discharged home on postoperative day #4. The presence of an accessory conduction pathway by itself does not carry any increased anesthetic risks, but the management of supraventricular tachyarrythmias that can result, have the potential for devastating outcomes. Management of WPW includes controlling the sympathetic nervous system in an attempt to avoid a hyperadrenergic state that may predispose these patients to SVT. Common medications used to control the heart rate in SVT may be detrimental in patients with WPW. Calcium-channel blockers such as verapamil or diltiazem, digoxin, and adenosine all slow conduction through the AV node2. These medications also may enhance conduction along the accessory bundle or at the very least do not slow conduction along this abnormal tissue, resulting in rapid ventricular rates. Once rapid conduction along the accessory bundle takes hold, a rapid ventricular response can deteriorate into ventricular fibrillation. The use β–blockers in patients with WPW may be useful in slowing re-entry tachyarrythmias through the accessory bundle1 as well as decreasing the sympathetic activation of the normal cardiac conduction pathways. Medications that directly increase circulating levels of catecholamines and the heart rate should be used with caution in patients with WPW. Management of these patients in the postoperative period continues to be crucial. Adequate pain results in decreased adrenergic output thereby lowering the possibility for tachydysrhythmia. Albeit, the incidence of WPW in the operating room is low, the potential for mismanaging the tachyarrythmias that can result are high and have the potential for devastating consequences. References: 1. 2. Gaita F, Giustetto C, Riccardi R, Brusca A. Wolff-Parkinson-White syndrome. Identification and management. Drugs.1992 Feb;43(2):185-200. German LD, Gallagher JJ. Functional properties of accessory atrioventricular pathways in WolffParkinson-White syndrome. Clinical implications. Am J Med.1984 Jun;76(6):1079-86.