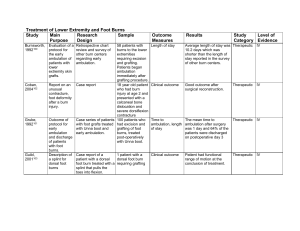
1 Table 1. Safety of Mobilizing Hospitalized Adults Author Study

Table 1. Safety of Mobilizing Hospitalized Adults
Author Study design Population Objective Conclusion
Medical
Bernhardt et al.
(2008)
Junger et al. (2006)
Prospective, open, randomized, controlledtrial, blinded outcome assessment
Stroke patients
(n=71)
To test whether a very early rehabilitation protocol, with a focus on mobilization, was safe and feasible to administer across multiple sites
No difference in safety measures between the standard care group and the early mobilization group among stroke patients.
Randomized study
DVT patients prescribed strict bed rest for at least five days (n=51), and DVT patients instructed to ambulate around the unit during the same five days
(n=52).
To evaluated the outcomes of pulmonary embolism, progression of thrombosis, nosocomial infections, serious events, and death between the best rest and ambulation groups
(13.5%) of the mobile group and (28.0%) of the immobile group developed at least one of the evaluated outcomes. No significant differences were found between those who ambulated and those who remained on bed rest, indicating that prescribing bed rest for this patient population is not a necessity.
Langhorne et al.
(2010)
Observerblinded, pilot randomized controlled trial
Stroke patients within 36 hours of symptom onset
(n=32).
To study the safety of early mobilization in patients hospitalized with an acute stroke
Stroke patients in the early mobilization group had no significant increase in falls, fatigue, or stroke progression compared to the control group, indicating the safety of early mobilization of acute stroke patients.
Trujillo-
Santos et al. (2005)
Observational study
Deep Vein
Thrombosis
(DVT) patients
(n=2,038) and pulmonary embolism (PE) patients (n=612)
Cardiac Procedure
To explore whether ambulation of acute
DVT and PE patients posed increased risk of developing new events of pulmonary embolism
There was no significant difference in the development of new PE, fatal PE, or bleeding complications between patients on bed rest and those allowed to ambulate.
Best et al. Prospective Left heart To determine the There was no difference in
1
(2010)
Boztosun et al.
(2007)
Butterfield et al.
(2000)
Chair et al.
(2007) nonconcurrent design with a retrospective control. catheterization
(LHC) sheath removal patients.
Traditional three- to four-hour ambulation protocol group
(n=402). 90 minute group
(n=193).
Observational Heart catheterization patients (n=1,650)
Quasiexperimental safety of ambulating patients at 90 minutes post-LHC sheath removal compared to the current practice of ambulation at three to four hours postsheath removal. complication rates for the two groups. The results suggest that early ambulation for selected patients at 90 minutes is safe
Observational study
Patients undergoing peripheral and renal angioplasty using a sheath size up to 6 French
(n=128)
To explore whether mobilizing selected patients after 2 hours of bed rest would increase vascular complications
To assess the incidence of puncture site compilations in inpatients undergoing early mobilization following angioplasty
Patients ambulated after 2 hours had less incidence of ecchymosis and small hematoma that those with longer periods of bed rest
(P<.001). it is both safe and feasible to ambulate selected patients at 2 hours following 6-French diagnostic left heart catheterization.
Mobilization at 4 hours after the procedure was successful in
90% of cases, while 10% required more prolonged bed rest at four hours.
Cardiac catheterization patients. (n=43) ambulated at 4 hrs post procedure &
(n=43) ambulated
12-24h after the procedure.
To compare patient outcomes of back pain, vascular back complications, and urinary discomfort between patients ambulated at 4 hours and 12–24 hours post-transfemoral cardiac catheterization
There was no difference between the two groups on vascular complications. The control group had significantly more back pain intensity (P <
.001) and higher levels of urinary discomfort (P = 006).
2
Dowling et al. (2002)
Prospective randomized study
Angiography patients randomized to group ambulating
To assess the feasibility and safety of early ambulation after transfemoral
No significant difference in hematoma formation, pseudoaneurysm development or other groin complications of
Gall et al.
(2006)
Prospective study
6 hours after procedure (n=47), and 3 hours after procedure (n=63) angiography patients ambulated at either 3 or
6 hours after catheter or sheath removal.
Coronary angiography patients (n=1,000)
To assess the safety of ambulating patients after 90 minutes of bed rest following coronary angiography
The 90 minute protocol was safe for patients undergoing elective 6-Fr coronary angiography performed via the right femoral artery.
Mah et al.
(1999)
Retrospective chart data
Cardiac catheterization patients, (n=472) in the 5-hour ambulation group and (n=408) in the
3-hour ambulation group.
To evaluate the effects of ambulating patients
3 hours after cardiac catheterization with a 7 French arterial catheter on bleeding, hematoma formation, and vascular complications
Patients who received the 3hour ambulation protocol experienced a significantly lower rate of bleeding and hematoma formation (13%) than patients who received the
5-hour ambulation protocol
(24.4%) (p < 0.001).
Ambulating patients 3 hours post cardiac catheterization with a 7F catheter was found to be safe.
Miracapillo et al.
(2006)
Randomized Pacemaker patients. (n=57) mobilized after 3 hours, (n=77) mobilized after 24 hours.
To test a new protocol mobilizing patients 3 hours after receiving a single or a dual-chamber pacemaker
No statistical differences were observed between the two groups
3
Rezaei-
Adaryani et al.
(2009)
Single-blind randomized controlled trial
Patients, who had undergone a nonemergency 6-
French cardiac catheterization via
To assess the effect of changing position and early ambulation on the amount of bleeding and hematoma after
The experimental group produced no significant increase in the amount of bleeding and hematoma when compared with the control group (P > 0.05).
Vlasic et al. (1999)
Prospective
Study the femoral artery
(n=70)
Cardiac catheterizaiton patients (n=50) cardiac catheterization.
To report the effects of reducing the 6 hour bedrest period to 2 hours following cardiac catheterization
No significant vascular complications occurred.
Vlasic et al. (2001)
Randomized controlled trial
Patients undergoing percutaneous coronary intervention randomly assigned to 2, 4, or 6 hours of bed rest (n=354)
To test if reducing the time to ambulation from 6 to
2 hours would not increase vascular complications
Reducing bed rest, after percutaneous coronary intervention, from 6 to 2 hours was safe and was not associated with an increased risk of vascular complications.
Walker et al. (2008)
Wang et al.
(2001)
Quasiexperimental
Percutaneous coronary intervention procedure patients
(n=338)
Quasiexperimental design
Left-heart catheterization patients (n=118) receiving 4 or 6 hours of bed rest
To explore groin complication rates of patients mobilized at
3, 4, and 6 hours after femoral arterial sheath removal following a percutaneous coronary intervention procedure.
To compare the effects of 4 hours of bed rest vs. 6 hours of bed rest on patients’ safety, comfort, and satisfaction levels
The length of bed rest after arterial sheath removal had no significant effect on bleeding
(P=0.21) or hematoma formation (P=0.612) at the groin puncture site for participants who mobilized at either 3, 4, or
6 hours after percutaneous coronary intervention arterial sheath removal.
No significant differences in arterial puncture site complications between mobilized at 4 hours versus 6 hours.
Surgical
Kaneda et al. (2007)
Observational
Retrospective
Lung cancer patients after a lobectomy. Group
1 encouraged to walk 4 hours after surgery (n=36),
To examine whether walking at 4h after surgery could be a safe approach to proceeding with rehabilitation.
No significant difference in the amount of drainage, rates of heart load during walking, pain scores, or falls. Results indicated that early mobilization at 4 hours after surgery was
4
Rath et al.
(2010)
Silvanto et al. (2004)
Whitney et al. (2004).
Randomized control trial
Randomized study
Randomized
Group 2 walked the day following surgery (n=50).
Foot drop patients who have undergone tendon transfer surgery.
Early active mobilization group
(n=13), immobilization group (n=11).
Knee arthroscopy patients (n=120) randomized into 3 groups:
Group E- early ambulation, Group
6-h – ambulation after 6 hours, &
Group L ambulation after
18-24 h
Explored whether the early active mobilization group would have similar rates of tendon insertion pullout compared to the immobilization group
Total hip replacement patients: (n=27) in standard treatment group, (n=31) in supplemental activity group feasible.
No cases of tendon pullout in either group, supporting the safety of early mobilization.
To evaluate the influence of ambulation time on the occurrence of transient neurologic symptoms (TNSs) after spinal anesthesia with 50 mg of 2% plain lidocaine for knee arthroscopy.
To test whether local tissue oxygen levels and wound healing responses in tissue close to the surgical wound of patients having total hip replacement were improved by early, supplemental postoperative physical activity.
TNSs developed in 3 patients
(7.5%) of Group E, in 11 patients (28%) of Group 6-h ( P
= 0.05), and in 5 patients (13%) of Group L. Early ambulation was not found to be a risk factor for transient neurologic symptoms after spinal anesthesia
Physical activity did not improve healing measures, however id did not reduce tissue oxygenation or wound healing
ICU
Bailey et al. (2007)
Prospective cohort study
ICU patients who had required mechanical ventilation for more than 4 days
(n= 103)
To explore whether early activity is safe and feasible for respiratory failure patients.
Early activity was both safe and feasible with a less than 1% occurrence of activity-related adverse events.
5
Bourdin et al. (2010)
Quasiexperimental
Stiller et al.
(2004)
Prospective study
ICU patients who had received invasive mechanical ventilation for 2 or more days (n=20)
Patients in the ICU for 7 days or more
& on mechanical ventilation for 2 or more days (n=31)
To explore the feasibility of early rehabilitation of ICU patients undergoing mechanical ventilation and the effects on common physiologic variables.
To measure the effects of mobilization on heart rate, systolic and diastolic blood pressure, percutaneous saturation of oxygen, deterioration in clinical status, and intervention required for it.
Early rehabilitation is feasible and safe in patients in the ICU for longer than 1 week. The most frequent contradictions were sedation (15%), shock
(11%), and renal support (9%).
Early rehabilitation was feasible and safe for this population based on physiologic variables studied. However, there were contraindications to the intervention, including sedation, shock, renal support, persistent respiratory failure, impaired response to simple orders, agitation, and confusion.
6