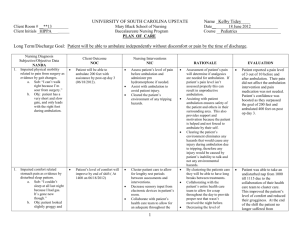
Length of Bed Rest and Rick of Bleeding Following Femoral
advertisement

EBP Project Abstract Appraised by: Michael Winegar SN, Cody Schumacher SN, Carson Winkels SN, & Garrett Mindt SN (NDSU Nursing at Sanford Health, Bismarck, ND) Clinical Question: In adults, does ambulating after 3 hours of bedrest following a femoral percutaneous coronary catheterization increase the risk of bleeding? Articles: Chair, S., Fernandez, R., Lui, M., Lopez, V., & Thompson, D. (2008). The clinical effectiveness of length of bed rest for patients recovering from trans-femoral diagnostic cardiac catheterization. International Journal Of Evidence-Based Healthcare (Wiley-Blackwell), 6(4), 352-390. Kobrossi, S., Tamim, H., & Dakik, H. (2014). Vascular complications of early (3h) vs standard (6h) ambulation post-cardiac catheterization or percutaneous coronary intervention from the femoral artery. International Journal of Cardiology. 176, 1067-1069. Mohammady, M., Heidari, K., Sari, A. A., Zolfaghari, M., & Janani, L. (2014). Early ambulation after diagnostic transfemoral catheterization: A systemic review and meta-analysis. International Journal of Nursing Studies, 51(1), 39-50. Tongsai, S., & Thamlikitkul, V. (2012). The safety of early versus late ambulation in the management of patients after percutaneous coronary interventions: A meta-analysis. International Journal Of Nursing Studies. 49(9), 1084-1090. doi:10.1016/j.ijnurstu.2012.03.012 Synthesis of Evidence: The systematic review by Tongsai and Thamlikitkul (2012) reviewed five studies. Of those studies, three articles were random control trials and two were non-randomized comparative studies. The design of the studies were to show that ambulating a patient two to three hours after a femoral PCI showed no increased risk for bleeding compared to waiting 6-10 hours. The findings were consistent through all five studies reviewed. The systematic review by Mohammady, Heidari, Sari, Zolfaghari, and Janani (2014) reviewed 20 randomized control trails. They examined the effects of the duration of bed rest after transfemoral catheterization on the prevention of vascular complications, general discomfort, pain, urinary discomfort and patient satisfaction. They results suggest ambulating patients 2-3 hours after transfemoral catheterization had no significant effects on the incidence of vascular complications. The systematic review by Chair, Fernandez, Lui, Lopez, and Thompson (2008) investigated seven randomized and quasi-randomized control trials on the effect of bedrest greater than 6 hours and less than 6 hours related to the incidence of bleeding. The findings demonstrated no statistically significant difference in the incidence of bleeding between the groups. The retrospective observational study done by Kobrossi, Tamim and Dakik (2014) observed the vascular complications rates among patients receiving PCI or CC and compared the incidence rates between patients who were ambulated 3 hours post op and 6 hours post op looking for an increase in complications among patients ambulated at 3 hours as opposed to 6 hours. The findings demonstrated no statistically significant increase in the rates of vascular complication occurrence among patients ambulated 3 hours post op compared to patients ambulated 6 hours post op. All of the articles showed these results to be consistent and did not increase the risk for bleeding. There was no evidence that early ambulation was more harmful than late ambulation in terms of a bleeding event. Bottom Line (findings): Early ambulation 2 to 3 hours after femoral catheterization does not increase the risk of vascular complications. It is shown to improve patient satisfaction and decrease length of stay. Implications for Nursing Practice: Nurses can implement early ambulation to improve patient satisfaction and decrease the incidence of vascular complications. The studies suggested that early ambulation is proven to be a safe and effective way to improve quality of care.