Ankle Ligament Reconstruction Pre Operative Education Program
advertisement

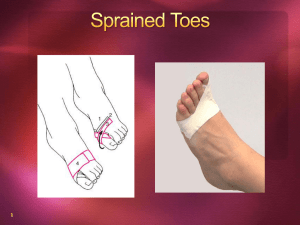
Ankle Ligament Reconstruction Pre Operative Education Program Prepared By Dr. Mark Glazebrook MD, MSc., PhD., FRCS(C) QEII HSC Daniela Rubinger BScPT, MCPA Citadel Physiotherapy Ltd. Introduction Ankle Ligament Reconstruction is a surgical treatment for chronic ankle joint instability designed to improve pain and function. For the patient to obtain the maximum benefit, it is important that they fully understand the ankle anatomy, reason for surgery, surgical procedure and rehabilitation process. This booklet will provide all necessary information to allow the patient to make an educated and thorough recovery from surgery. Ankle Anatomy The hindfoot has two joints; the ankle joint and the subtalar joint (Figure 1). The ankle joint is composed of 3 bones, the tibia which forms the superior and medial, portion of the ankle; the fibula which forms the lateral, and the talus which forms the inferior portion of the ankle joint. The ankle joint is responsible for up and down motion of the foot. Beneath the ankle joint is the second part of the ankle, the subtalar joint, which consists of the talus on top and calcaneus on the bottom. The subtalar joint allows side to side motion of the hindfoot foot. The ends of the bones in these joints are covered by articular cartilage. The articular cartilage provides a cushioned surface for the bones of the ankle joint to slide by each other during foot up and down movement. There are many major ligaments of the ankle which connect the tibia to the fibula on the front of the ankle, the fibula to the calcaneous on the outside of the ankle and the tibia to the talus and calcaneous on the inside of the ankle. These ligaments provide stability to the ankle. Ankle Sprain Ankle sprains commonly occur when the ligaments are stretched more than normal resulting in a partial or complete tear of the ligament. This ligament damage results in abnormal excessive movement in the ankle due to loss of ankle stability. Ankle Sprains can be sprains are divided into several groups depending on the severity of damage to the involved ligament. Grade I Sprain - A Grade I (First Degree) sprain is the most common. The ligaments are over-stretched, and damaged microscopically, but not torn. The ligament damage has occurred without any significant instability developing. Grade II Sprain - A Grade II (Second Degree) injury is more severe and indicates that the ligament has been more significantly damaged, but there is no significant instability. The ligaments are often partially torn. Grade III Sprain - A Grade III (Third Degree) sprain is the most severe. This indicates that the ligament has been significantly damaged, and that instability has resulted. A grade III injury means that the ligament has been torn. Ankle Instability Ankle injuries are extremely common, and the vast majority of ankle sprains recover fully within six weeks of injury. Occasionally, if the ligaments are severely disrupted, patients may suffer weakness or giving way of the ankle beyond this period. What are the symptoms? Most people with ankle instability complain of one or more of the following: - The ankle gives way on uneven ground, playing sport or even just walking - Pain with each episode, which recovers quickly - Feeling of instability or weakness in the ankle - Swelling or puffiness Surgical Procedure Mark to do…. Rehabilitation Process Rehabilitation following ankle ligament reconstruction surgery should begin prior to the surgery with the education of the client and proper preparation to ensure that everything is in place for a successful rehabilitation process. Important things to consider: You will be encouraged to attend a Pre-operative Physiotherapy appointment. This will consist of a session in which the physiotherapist will educate you on the surgical procedure and the rehabilitation process. Prior to the surgery you will also be fitted with a walking cast called a boot walker (Figure 3). This specific type of ankle brace will be required to be worn for the first 6-8 weeks post surgery. You will be non-weight bearing for the first 2 weeks so you will require crutches for mobility. Polar Care Unit It maybe possible to use this during the initial two weeks post op. Let me know what you think. Cast Boot/ Boot Walker Figure 3 The cast boot is designed to immobilize the foot and ankle and lower leg while allowing safe ambulation. The reinforced nylon shell provides maximum rigidity while the wrap around liner with Velcro straps provides comfort. There is a large rocker bottom for improved weight transfer during gait. Post Operative Protocol The following protocol has been developed for the post – operative rehabilitation of the Ankle Ligament Reconstruction patient. Week 1-2 Goals - Rest and recovery from surgery - Control swelling and pain - Increase ADL General Considerations - NWB in boot - Sutures removed at approximately 10 days - Encourage ADL - Rest and elevation to control swelling - Control pain - Hip and knee range of motion exercises Week 3-6 Goals - Allow healing while maintaining upper body, core, hip and knee strength and ROM Protocol - FWB in walker boot at all times - Massage for swelling Elevation to control swelling Gentle AROM ankle PF/DF/eversion and toe flexion/extension Stationary bicycle with boot Core exercises – abdominal recruitment, bridges on ball, arm pulleys/theraband diagonal patterns Hip AROM and strengthening (clam, side lift, glut max. SLR) Knee AROM and strengthening ( SLR, theraband press or leg press machine) Stretching – Glut max, glut. Med, piriformis, erectus femoris, hamstrings Week 7-10 Goals - WB in boot with pain and swelling control Protocol - WB in boot - Stationary bicycle - AROM – begin inversion and eversion; continue with PFDF, toe flex/ext. - Continue with core exercise, hip strengthening and knee strengthening exercises. Progress to standing. - Manual mobilizations to joints not part of ligament reconstruction Week 11-12 Goals - Full ROM Protocol - Wean from boot walker - Control swelling and pain with elevation and modalities as needed - AROM in WB - Manual mobilizations as required - Muscle stimulation to intrinsics, invertors/evertors if required. - Gait retraining - Continue strengthening core, hips and knees - Proprioceptive training – balance board, uneven surfaces, etc. Week 13-16 Goals - Full ROM in WB - Good single leg stance - Near full strength in lower extremity Protocol - Proprioceptive training o Single leg stance on uneven surface with resistance to arms or NWB leg o Double stance on balance board, Sissel, Fitter o Single leg WB on balance board, Sissel, Fitter - o Single leg WB on balance board, Sissel, Fitter with resistance to arms NWB leg Strength – toe raises, lunges, squats, hopping, skipping, running at approximately 14 weeks Manual mobilization if required Week 16+ Goals - Full functional return to work and or activity Protocol - Continue to build endurance - Work specific or activity specific retraining - Pylometric training