ppt - Stewart Morrison
advertisement

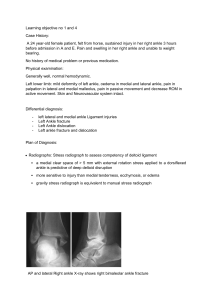
Robert B. Anderson, MD Kenneth J. Hunt, MD Jeremy J. McCormick, MD Management of Common Sports-related Injuries About the Foot and Ankle J Am Acad Orthop Surg 2010;18: 546-556 Stewart Morrison Orthopaedic Registrar Western Health June 2011 Robert B. Anderson, MD Kenneth J. Hunt, MD Jeremy J. McCormick, MD Management of Common Sports-related Injuries About the Foot and Ankle J Am Acad Orthop Surg 2010;18: 546-556 Stewart Morrison Orthopaedic Registrar Western Health June 2011 Outline ✚ Incidence ✚ Evaluation ✚ Specific Injuries ✚ Turf Toe ✚ Ankle Injuries ✚ Tarsometatarsal Injury ✚ Stress Fracture ✚ Prevention Incidence ✚ NCAA Injury Surveillance System (ISS) ✚ Hootman et al. reported on 16 year data for 15 sports: ✚ Ankle ligamentous sprains most common: 14.9% of injuries, 0.83 per 1000 athletes ✚ Anterior cruciate ligament injuries: 2.6% of injuries, 0.28 per 1000 athletes ✚ High school level, ankle and foot constituted 39.7% of athletic injuries ✚ Games of the XXVIII Olympiad Athens, 22% of injuries were ankle sprains ✚ Sport Factors ✚ Base Sliding (breakaway bases) ✚ Football (American) has highest injury rate Evaluation ✚ Mechanism of Injury ✚ “return to play” as an important issue ✚ Have injury prevention strategies been followed? ✚ Temporal issues “the goal is not simply to return to participation, but to perform at a high level while avoiding long-term consequences.” Turf Toe ✚ Hyperextension 1st MTP joint ✚ Tearing of plantar capsuloligamentous structures ✚ Commonly associated valgus component Hx: 1st MTPJ pain/swelling, push-off / cutting Ex: 1st MTPJ stability, hallux flexion strength Ix: AP XR: Excl. sesamoid #, proximal migration Turf Toe I : attenuation, swelling, minimal ecchymosis ✚ Non Surgical: taping, early rehabilitation II : partial tear, moderate swelling, restricted ROM ✚ Non Surgical: 2 weeks rest, taping ✚ “turf-toe” or carbon-fibre orthosis to prevent MTP extn. III : Complete disruption, FH weakness, instability ✚ Non Surgical: Immobilisation 10-16 weeks ✚ Surgical: Open Repair of Capsule case series of 19 athletes, 17 returned to previous level of participation. Ankle Inversion ✚ Inversion most common injury ✚ ATFL, PTFL, FCL ✚ “more extensive evaluation may be indicated when a severe sprain arouses suspicion of a fracture or in cases in which symptoms fail to resolve within 4-6 weeks” ✚ High incidence of peroneal nerve neuropraxia DDx: ST Dislocation, # Ant. Process Calcaneus, Avulsion base 5th MT Ankle Inversion I : stretched lateral ligament. Able to WBAT without crutches. II : Partial tear of ligament. Able to walk several steps unassisted. III : Complete tear. Feeling of instability and difficulty walking. ✚ Most managed non-surgically. ✚ Several treatment algorithms exist, most incorporating RICE, early mobilisation and strengthening, +/- taping. ✚ Return to activity in 6-8 weeks. ✚ MRI Evaluation ✚ Complete treatment of initial injury, peroneal strength, and proprioceptive activities, decrease change of recurrent injury or chronic instability. Ankle Eversion ✚ Risk of injury to the tibiofibular syndesmosis ✚ Predictive of longer recovery and residual symptoms ✚ Valgus, external rotation, eversion ✚ +/- MCL Knee ✚ “Squeeze Test”, External Rotation Test ✚ MRI: Syndesmotic or FHL oedema static evaluation Ankle Eversion Stable (No Widening) ✚ CAM Boot until non-tender, graduated return to activity at that point. ✚ ~ 6 weeks recovery time ✚ “15 hops on affected leg” good indicator of appropriate return to sport. Unstable (Widening) ✚ Sydesmotic Fixation ✚ Open vs. closed vs. suture button ✚ Author’s preferred method is plate, screw, and button, with screw removed at 10-12 weeks. ✚ Plate to protect against fracture through empty screw hole. TMT (Lisfranc) Injury ✚ Axial loading mechanism ✚ Often Missed: often ligamentous, subtle clinical and radiographic findings Dx: “pop” in midfoot, rapid onset pain. Tender on midfoot compression, pronation, supination, stressing 1st ray into dorsal or plantar deviation relative to second metatarsal head. XR: B/L WB AP, 30° Oblique, Lateral ✚ > 2mm between 1st and 2nd metatarsal bases, fleck sign ✚ Stress views if plain radiographs equivocal MRI: not indicated if diastasis seen on plain film TMT (Lisfranc) Injury Sprain : Non-displaced, stable midfoot on stress radiographs ✚ Non-Surgical Management Rupture/Avulsion : Diastasis > 2mm (compared to other foot) on stress XR ✚ Principle: Obtain and maintain anatomical reduction of the midfoot ✚ Screws: Medial Cuneiform to 2nd MT, 1st/2nd MT-Cuneiform Screws ✚ Dorsal Plating: No disruption of articular surface ✚ Suture Button: little evidence ✚ Recommendation against using K-wires ✚ Strict NWB 6 weeks, early active mobilisation, arch support @ 6/52 , return to sport at 4/12 - 1yr ✚ Removal of hardware controversial Stress Fracture ✚ Most common overuse injuries in athletes, tibia and foot overrepresented ✚ Associated with change in training intensity, program, footwear, running surface ✚ Related to repetitive load ✚ Higher risk with forefoot or hindfoot varus ✚ Dx: Point tenderness, -ve XR ✚ Tc99 Bone Scan vs. MR, then CT ✚ High Risk: 5th MT metaphyseal, medial malleolar, navicular, anterior tibial cortex ✚ Mx: Immobilization, Boot, ProtWB 6-8 weeks. Maintain non-impact activities. Nutrition. ✚ Recent data to suggest surgical management appropriate Prevention ✚ Continued injury surveillance, awareness, and innovation ✚ Footwear: Insoles, high-top shoes ✚ Playing Surfaces: Artificial Surfaces + Cleats ✚ Performance (high traction coefficient) vs risk (excessive torque) Reflection ✚ Foot and ankle injuries are common ✚ Sport and mechanism specific ✚ Patient demographics, function, comorbidities critical in determining management, as well as critiquing literary evidence