DISEASES OF THE BLOOD VESSELS: DEGENERATIVE
advertisement

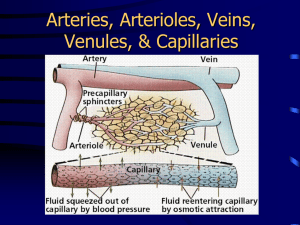
1 DISEASES OF THE BLOOD VESSELS Clinical manifestations of blood vessel diseases. -pathologic changes in blood vessels have one or more basic consequencies narrowing of the lumen of the vessel (vascular atrophy), occlusion of vessel (tissue ischemia), and potential infarction in tissues supplied by the vessel damage to the intima with thrombosis weakening of the wall with dilatation (aneurysm) and/or potential rupture of the blood vessel Congenital anomalies of blood vessels. 1- berry aneurysm- caused by congenital focal weakness of the blood vessel wall results in outpouching -occur in cerebral vessels- weakening of the wall may lead to fatal rupture- resulting in subarachnoidal hemorrhage 2- arterio-venous fistula- is an abnormal communication between vein and artery -may be congenital or caused by trauma -fistulas may cause left-to right shunt with an increase of venous return - possible right heart failure -may cause fatal hemorhage ACQUIRED DEGENERATIVE DISEASES OF BLOOD VESSELS. ARTERIOSCLEROSIS -is slowly progressive disease of arteries, characterized by thickening and loss of elasticity of arterial walls atherosclerosis - is a slowly progressive d. of arteries characterized by elevated intimal fibrofatty plaques, formed by lipid deposition, smooth muscle proliferation and synthesis of extracellular matrix - large to medium-sized muscular arteries and large elastic arteries are involved, particularly the aorta, and its branches, coronary arteries, and arteries of the circle of Willis arteriolosclerosis -affects small arteries and arterioles -occurs in two variants, as hyaline and hyperplastic, both cause thickening of the vessel wall with luminal narrowing hyaline arteriolosclerosis- is characterized by diffuse pink hyaline thickening of the aretriolar wall 2 -occurs typically in older pateints - affects the kidney- causes benign nephrosclerosis - grossly: - the kidneys are symmetrically atrophic, finely granular surface microscopically: - hyaline thickening of the walls of the small arteries and arterioles (homogenous, pink) with narrowing of the lumena - decrease of the blood flow through affected vessels- causes ischemia and ischemic atrophy of the kidney - in younger patients- associated with arterial hypertension and DMfrequency and severity of the lesions is increased hyperplastic arteriolosclerosis -characteristic of malignant hypertension- microscopically- concentric lamellar „onion-skin“ arteriolar thickening with reduplication of basement membrane and smooth muscle cell proliferation- fibrin deposition and vessel wall necrosis ATHEROSCLEROSIS - is the most important pattern in arteriosclerosis pathogenesis and epidemiology: multifactorial, idiopathic, not completely understood risk of development of atherosclerosis increases with -age, cigarette smoking, positive family hypertension, diabetes mellitus, and hypercholesterolemia history, -major acquired risk factors: 1) acquired hyperlipemia 2) hypertension 3) cigarette smoking 4) diabetes mellitus -the risk is correlated with elevated serum levels of low-density lipoprotein (LDL) -the higher total cholesterol level, the greater risk of AS pathogenesis: - most theories invoke some damage to endothelium or underlying smooth muscle with subsequent proliferation of smooth muscle cells "response-to-injury-hypothesis" - according to this idea- atherosclerosis is a reaction to chronic repeated endothelial cell injury, caused by such insults as hyperlipidemia, hypertension, cigarette smoking, diabetic 3 microangiopathy, circulating endotoxins, anoxia, hypoxic changes, viruses, turbulent blood flow,etc. -endothelial injuries induce metabolic and structural changes accompanied by increased permeability to plasma constituents, such as lipids, lipoproteins, mainly cholesterol - these substances may accumulate within the intima at these sites of endothelial injurybecause of local increase of endothelial cell permeability -subsequent cellular events include imigration of macrophages into the intima- these change to foamy cells -endothelial injury also result in adhesion of platelets and monocytes and release of factors from activated platelets and monocytes, such as PDGF- platelet-derived growth factor, induce smooth muscle proliferation and their migration to the intima, -smooth muscle cell produce large amounts of extracelular matrix components, such as collagen, elastic fibres, proteoglycans -smooth muscle cells accumulate lipid (cholosterol) to become foam cells MORPHOLOGY OF ATHEROSCLEROTIC LESIONS 1) FATTY STREAKS -are thin flat yellow streaks in the intima- caused by lipid depositions in the cytoplasm of intimal mesenchymal cells and in macrophages- aggregates of foamy cells -they may occur in the aorta very early in life- are harmless and reversible in early stage- there is not a obvious relation to AS- some of them disappear, some may progress to atheromatous plaques- many believe however that fatty streaks are precursors of AS plaques 2) ATHEROMATOUS PLAQUES- fibrofatty atheroma - fibrous plaques -early changes- monocytes adhere to endothelial cells close to the site of injurymigrate between endothelial cells to get to the subendothelial spacethan change to foamy cells - in addition- smooth muscle cells from the media layer- become larger and proliferate- these cells also take up lipids to form foam cells- aggregates of foam cells within the intima = fatty streaks -later plaque) stage-MATURE FIBROFATTY ATHEROMAS (intimal -is composed of aggregates of foam cells and macrophages and SMCs, extracellular lipids, cellular debris, fibroblasts and collagenous matrix -with proggresion of the disease- fibrofatty atheroma is modified by further deposition of collagen, elastin, proteoglycans. Atheromas 4 undergo considerable cellular proliferation and formation of fibrous connective tissue = FIBROUS PLAQUES -secondary changes in atheromatous plaque-dystrophic calcification-very common -severely affected vessels- can be changed into completely calcified rigid tubes -ulceration of the overlying endothelium - thrombosis of the plaque- most common complication -thrombosis- often associated with ulceration -parts of atherothrombotic masses- may be discharged to the blood stream as emboli -vascularisation of the plaques- may lead to the hemorrhage in the plaques- occlude the lumen (coronary vessels) -aneurysms may develop in vessels weakened by extensive plaque formation- the abdominal aorta is a favourite site HYPERTENSIVE VASCULAR DISEASE -hypertension is the single most important risk factor in both coronary heart disease and cerebro-vascular accidents -it may also lead directly to congestive heart failure (hypertensive heart disease), to renal failure and aortic dissection -90% of hypertension is primary and idiopathic- essential hypertension-10% of hypertension is secondary-mostly related to renal disease, endocrine abnormalities, vascular malformation blood pressure- is a complex trait that is determined by the interaction of multiple genetic and environmental factors that regulate the relatioship between cardiac output and total arteriolar resistence pathogenetic mechanisms leading to essential hypertension-essential hypertension is either related to a primary increase in cardiac output (retention of natrium) -or to an increase in peripheral resistence- release of vasoconstrictive factors, neurogenic causes, increased sensitivity of smooth muscle cells, etc. Inflammatory Diseases of Blood Vessels. 1) POLYARTERIITIS NODOSA =systemic disease characterized by necrotizing inflammation of medium- and small-sized arteries throughout the body sparing the pulmonary circulation -most often - in middle aged adults, more often in males 5 -disease is characterized by fibrinoid necrosis of the intima, and heavy mixed inflammatory infiltration in and about the vessel- infiltrates composed of lymphocytes, plasma cells and leukocytes -vasculitis in acute phase is characterized by transmural inflammation composed of neutrophils, eosinophils frequently associated with fibrinoid necrosis of the inner half of the vessel wall -lumen becomes thrombosed- results in acute tissue ischemia and infarction - in later stage- nodular fibroblast proliferation and irregular aneurysmal dilatation of blood vessels Clinical course: virtually all organs may be affected with exception of the lungs, most commonly affected- are kidney, heart, liver, GIT - variety of clinical symptoms including malaise= vague feeling of physical discomfort, fever, weakness, weight loss -renal involvement- possible cause of death - vascular lesions of the GIT- abdominal pains, diarrhea, melena - peripheral neuropathy 2) WEGENER'S GRANULOMATOSIS = is characterized by complex of three major symptoms 1) necrotizing granulomas of the upper respiratory tract and 2) necrotizing or granulomatous vasculitis of small arteries and veins most commonly in the lungs and 3) necrotizing glomerulonephritis pathogenesis: no etiological agent has been identified -immune complexes are occasionally present in vessell walls and glomeruli, most patients have antineutrophilic cytoplasmic autoantibodies ANCA clinical symptoms: the course of untreated disease - is progressive diagnosis: - biopsy of upper respiratory tract lesions appropriate therapy: prednisone+ antibiotics 3 ) THROMBANGIITIS OBLITERANS ( BUERGER'S DISEASE) =is a chronic relapsing inflammatory vascular disease characterized by acute and chronic vasculitis of medium-sized and small arteries followed by thrombosis of affected vessels and severe vascular insufficiency -mostly affected- arteries of lower extremities- may lead to gangrene pathogenesis: unknown, but closely related to the use of tobacco products -tobacco smoking (clear mechanism is not established yet) 6 leads to endothelial damage- either direct toxicity or it initiates immune reaction morphology: -arterial walls are infiltrated by mixed inflammatory cells, mostly lymphocytes, the lumen is closed by thrombosis -thrombus typically contains small microabscesses- inflammatory reaction may extend to acompanying veins and nerves (organization of thrombi) clinical symptoms: claudications, color and temperature changes in lower extremities -chronic ulcerations of the toes, feet, fingers- gangrene, severe pain even at rest -stop of cigarette smoking-relief from further attacks 4 ) RAYNAUD'S DISEASE =paroxysmal pallor or cyanosis of acral parts (fingers, tip of nose, ears) caused by intense spasm of small arteries and arterioles -idiopathic disease in young women -in contrast, Raynaud syndrome refers to arterial insufficiency of acral parts caused by some other disorders, such as atherosclerosis, Buerger disease, vascular disease in lupus erythematodes in later stage- trophic changes, ulcerations in the skin, areas of gangrene in finger tips 5) LEUKOCLASTIC ANGIITIS -disease involves small vessels than PAN, lesions are characterized by fibrinoid necrosis and rich lekocytic infiltration within the affected blood vessel wall -pathogenesis: immune complexes in previously sensitized person, intiated by drugs, microorganisms, heterologous protein, etc ANEURYSMS = abnormal focal dilatation of arteries or veins -develop wherever there is marked weakening of the wall of the vessel most common causes of aortic aneurysms -atherosclerosis, cystic medionecrosis other causes -inflammatory-syphilis -congenital (intracranial arteries)accidents may lead to cerebrovascular 7 -traumatic -mycotic- due to local inflammation 1) atheroclerotic aneurysms- is by far the most common, mostly affected- abdominal aorta -AS aneurysms take form of saccular or cyllindroid swelling -mural thrombus is frequently found within the aneurysmal sac clinically: -parts of thrombus from the aneurysm may embolize -occlusion of renal, mesenteric or other arteries may result from the pressure in the aneurysmal sac -rupture- rare in smaller, very often in larger than 6 and more cm in diameter dissecting aneurysm = special type of aneurysm, characterized by the intima defects that allows the blood to penetrate into the aortic wall with propagation of hemorhage along the vessel clinically: - severe chest pain, abdominal pain due to compresion of mesenteric arteries, and sudden decrease of blood pressure treatment: - immediate administration of antihypertensive drugs -replacement of the affected part of the aorta by the graft morphology: -longitudinal tears in the intima of the aorta (sharp, irregular edges) -blood enters through the intimal defect into the media- hematoma -typically devides the outer and middle thirds of the aorta -the hemorhage may dissect in proximal direction to the heart or to the periphery -in about 20%- focal areas of degenerative changes in the media known as cystic medionecrosis Erdheim (may be a part of Marfan syndrome) VENOUS DISEASES two most important diseases- varicose veins and phlebothrombosis 1) VARICOSE VEINS - abnormally dilated tortuous veins -varicose change is caused by higher pressure in the venous lumen -most commonly affected- superficial veins of the leg 8 causes: -degenerative changes in vessel walls, muscle atrophy, intraluminal pressure -higher -familial tendency morphology: -affected veins are dilated, tortuous and elongated, focal thickening of the blood vessel wall -common complication- phlebothrombosis special types of venous varicosities: 1) hemorrhoids- result from varicose dilatation of the hemorhoidal plexus of the vein at the anorectal junction- bleeding to GI- melena 2) varicose veins in the esophagus- in patients with portal hypertension- due to liver cirhosis- rupture may cause death clinically: -lower extremities varicose veins- usually asymptomatic, rarely pain, but often followed by thrombosis of the venous plexuses Thromboembolic disease: -thrombi most common- in deep veins of the lower extremitiessource of pulmonary embolism TUMORS OF BLOOD AND LYMPHATIC VESSELS benign-benign vascular tumors frequently are seen in skin are very common-most 1) capillary hemangioma -most common sites - skin, membranes of oral cavity and lips, subcutaneous tissue, mucous less common sites- spleen, liver, salivary glands, etc. -grossly: bright red or bluish lesions, may level with the surface or may be elevated -usually present at birth, may regress spontaneously -morphology:- composed of capillary-like endothelial cells and filled by blood or lymph, channels lined by -these channels are separated one from another by a scant connective tissue stroma -thrombosis or fibrous organisation in the lumina- common 9 2) cavernous hemangioma -occurence - skin, subcutaneous tissue, internal organs, such as spleen, liver, pancreas 3) multiple vascular tumors in cerebellum, brain stem and internal organs- associate in clinical syndrome called von HIPPEL-LINDAU DISEASE (VHL gene mutated) borderline malignancy 1) epithelioid hemangioendothelioma -is an angiocentric vascular tumor with metastatic potential, composed of epithelioid endothelial cells arranged in short cords and nests in myxohyaline stroma Sites of involvement: the tumor develops in deep soft tissue of extremities, less commonly in bone, liver and lungs Clinical features: the tumor develops painful nodule-behaviour is intermediate with an uncertain clinical course-it is locally aggressive, recurrence rate is 10-15%, metastatic rate about 25% malignant 1) Angiosarcoma- is a rare malignant tumor the cells of which recapitulate the features of endothelium - cutaneous tumors in old patients, affect the skin of head and neck region, less commonly soft tissues are affected clinically- are highly aggressive tumours- local recurrences develop in 30%, one half of patients are expected to die of tumour within one year after diagnosis with metastases in the lungs, bone, lymph nodes, soft tissues, etc. 2) KAPOSI SARCOMA KS is a locally aggressive endothelial tumour that typically presents with cutaneous lesions in the form of plaques, nodules, pathes but may also involve mucosal sites, lymph nodes and visceral organs, earlier- it was a rare tumor, now more common- in immunosupressed patients and particularly important- in AIDS