Table 1. Studies of the safety and efficacy of propofol administered
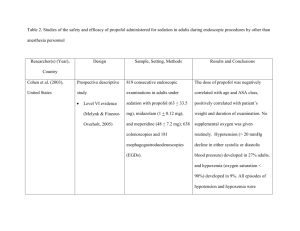
advertisement

Table 1. Studies of the safety and efficacy of propofol administered for sedation in adults and children by an anesthesiologist, nurse anesthetist, or assisting physician not directly involved with the endoscopic procedures Researcher(s) (Year), Design Sample, Setting, Methods Results and Conclusions Amornyotin et al. Randomized controlled 170 adults; high risk patients were The researchers concluded that in the (2007), Thailand trial (RCT) excluded from both groups. adult Thai population, sedated diagnostic Control group (C) received topical esophagogastroduodenoscopy (EGD) led Country Level II evidence (Melynk & Fineout- pharyngeal anesthesia alone. Overholt, 2005) to increased patients’ and endoscopists’ Intervention group (I) received satisfaction and increased patient topical pharyngeal anesthesia and willingness to repeat procedure in the intravenous sedation with future if needed. midazolam maintained with The researchers did not provide procedure continuous propofol infusion. times for either group, but did comment that the control group (unsedated patients) moved through the endoscopy unit faster. Hypertension and tachycardia were the most common complications in the control group and hypotension was the most common complication in the intervention group. The severity of complications was not reported. Barbi et al. (2003), Italy Prospective descriptive 1,059 invasive procedures in Major desaturation requiring a short study children birth to 20 years of age course of ventilation occurred 0.8% Level VI evidence (i.e., colonoscopy; EGD; lumbar children undergoing EGD, 0.3% children (Melynk & Fineout- puncture; bone marrow aspiration; undergoing painful procedures, and 0% Overholt, 2005) liver, muscle or skin biopsy; children undergoing colonoscopies. arthrocentesis; intestinal washout; Laryngospasm occurred in 2.1% children. and paracentesis) performed in a No children required intubation. The pediatric ward of a tertiary-care researchers concluded that the use of pediatric teaching hospital. propofol with concurrent oxygen administration allowed sedations in children with no significant complications for colonoscopies and painful procedures; however, the complications in children undergoing EGD were too high for recommending use of propofol for sedation in a unit with residents in attendance. Disma et al. (2005), Double-blind RCT 240 ASA class I –II children, 1-12 Five patients in Group P were treated with Italy Level II evidence years of age, undergoing bag-and-mask ventilation for < 1 minute. (Melynk & Fineout- diagnostic EGD were given Recovery time and discharge from the Overholt, 2005) midazolam as a premedication and hospital were similar in the three groups. then were randomly assigned to There was a lower incidence of adverse one of three groups—propofol events in Group PM and in Group PF than alone, three 1 mg/kg doses (Group in Group P (p < 0.05). The researchers P); same doses of propofol and concluded that propofol in combination fentanyl 1 mcg/kg (Group PF); or with fentanyl or midazolam gives better the same doses of propofol and sedation and ease of endoscopy than midazolam 0.1 mg/kg (Group propofol alone. PM). Additional doses of propofol were given during the procedure in all three groups as needed. All medications were administered and children were monitored by an anesthetist. All children received 3 L/minute oxygen per nasal cannula. Fanti et al. (2004), Italy Prospective descriptive 205 adults undergoing endoscopic The quality of sedation was judged study retrograde satisfactory for 98% by both the Level VI evidence cholangiopancreaticography endoscopist and the nurse assistant. (Melynk & Fineout- (ERCP) were sedated by an Hypoxia (oxygen saturation < 85%) Overholt, 2005) anesthesiologist using a propofol occurred in 1.9% of ASA Class III or target-controlled infusion system. higher patients, responding to either The target plasma concentration of turning patient to the supine position to propofol ranged from 2-5 mcg/mL. improve airway patency or manual A bolus of fentanyl (50-100 mcg) ventilation for a few minutes. Mean time was administered if signs of to discharge was 31 + 12 minutes post- insufficient analgesia were procedure. The researchers concluded that observed at the maximum target a target-controlled infusion system for concentration of propofol allowed. administration of propofol provides safe and effective sedation during ERCP. Khoshoo, Thoppil, Two parts: retrospective There were two groups: 155 The onset of sedation was faster (p < 0.01) Landry, Brown, & Ross descriptive study consecutive children (0.2-17.7 and the length of the procedure and (2003), United States involving 200 children years of age) underwent diagnostic recovery was significantly shorter (p < and a prospective RCT EGD received sedation with 0.01) in the PM group in both the involving 60 children. propofol with or without bolus retrospective and prospective parts of the Levels VI and II premedication with midazolam study. In the retrospective part of the evidence, (PM group); data were collected study, an equal number of children in both respectively retrospectively in 125 and groups required increased supplemental (Melynk & Fineout- prospectively in 30 children. 105 oxygen or transient use of bag-valve-mask Overholt, 2005) consecutive children received ventilation. In the prospective part of the sedation with bolus midazolam for study, more children in the MM group induction and maintenance as required increased supplemental oxygen. needed plus meperidine at No child required bag-valve-mask induction only (MM group); data ventilation in the prospective part of the were collected retrospectively in study. The researchers concluded that 75 and prospectively in 30 propofol is safe and effective for children. facilitating diagnostic EGD in children. All procedures occurred in the pediatric intensive care unit with the intensivist administering all medications. All patients received l L/minute of supplemental oxygen via nasal cannula. Seifert et al. (2000), Double-blind RCT 239 adults, equally divided During therapeutic endoscopy, sedation Germany Level II evidence between those undergoing with midazolam and propofol requires a (Melynk & Fineout- therapeutic EGD and those lower total dose of propofol, but otherwise Overholt, 2005) undergoing ERCP, were randomly has no superior sedation efficacy and is assigned to receive either propofol associated with a slower post-procedure alone (Group A) or midazolam and recovery than sedation with propofol propofol (Group B). alone. Anterograde amnesia for the procedure was present for all cases. Retrograde amnesia was present for ~ 25% of cases in both groups. Tosun et al. (2007), Double-blind RCT; Ninety ASA I-II children aged 1- Sedation was achieved in all procedures, Turkey 16 years old. and all but one (due to laryngospasm) was Level II evidence (Melynk & Fineout- Propofol-ketamine (PK) compared Overholt, 2005) successfully performed. Major with propofol-fentanyl (PF) for desaturation (10 seconds of apnea or SaO2 sedation in children undergoing < 85%), requiring a short course of EGD. ventilation using bag-and-mask with Additional propofol (0.5-1 mg/kg) supplemental oxygen, occurred in 0.8% was administered when a child children undergoing EGDs and 0.3% showed discomfort in both groups. undergoing colonoscopies. Laryngospasm Supplemental oxygen 3-4 (stridor), requiring use of bag-and-mask L/minute was given via nasal with oxygen supplementation or cannula in all children. continuous positive airway pressure ventilation, occurred in 2.1% of children undergoing EGD. The researchers concluded that both the PK and PF combinations provided effective sedation in children, but the PK combination resulted in stable hemodynamics and deeper sedation although more children experienced side effects. Vargo et al. (2002), Double-blinded RCT 75 adults ASA Class I-III received Adults receiving propofol had shorter United States Level II evidence either gastroenterologist- recovery times (18.6 versus 70.5 minutes, (Melynk & Fineout- administered propofol or p < 0.001) and a higher recovery of both Overholt, 2005) meperidine/midazolam for ERCP baseline activity level and dietary intake or endoscopic ultrasonography. 24 hours after the procedure (71% versus Monitoring with capnography 43%, p = 0.028). If a registered nurse had allowed for rapid titration of administered the propofol, the cost would propofol at the earliest signs or have been $59.80 versus $66.80 for respiratory depression. meperidine and midazolam, making Supplemental oxygen was not propofol more cost effective. Thus, the given routinely. A dedicated researchers concluded that gastroenterologist administered the gastroenterologist-administered propofol bolus doses of sedation and using monitoring with capnography is monitored the patient. similar to meperidine/midazolam for both physiological outcomes and patient/endoscopist satisfaction and leads to significantly improved baseline activity and food intake 24 hours later.