Clinical Decision Making In Emergency Medicine LLSA Review 2009
Are antibiotics Necessary After Incision and Drainage of a
Cutaneous Abscess?
Ann Emerg Med 2007;50:49-51
Clinical Decision Making In Emergency Medicine LLSA
Review 2009
Ehsan Shirazi, M.D.
• Publication: Annals of Emergency Medicine
• Design: Systemic Review
• Authors: Abigail Hankin MD & Worth Everett, MD
• Site: Department of Emergency Medicine, University of
Pennsylvania
Objective
• To determine whether oral antibiotics are necessary after incision and drainage of simple abscesses
• Concerns: antibiotic misuse, antibiotic resistance, and the emergence of MRSA
Introduction
• Cutaneous abscesses are common in adult and pediatric ED populations
• Simple abscesses are treated with or without oral antibiotics
• Infectious Disease Society of America and Center for Disease
Control recommend I&D alone
– Exceptions: Recurrent or persistent abscesses which then require antibiotics
Methods
A. Authors searched Ovid MEDLINE from 1966 to the present and
EMBASE from 1980 to present
B. They also examined bibliographic references in the most relevant articles and a secondary PubMed related article search
C. Primarily 1396 articles found; then by limiting the results to human subjects and English language 789 articles obtained
D. Both authors reviewed all the articles with the focus on original published research article that specifically addressed the utility of antibiotics after I&D of an abscess
Results
•
They identified 5 original research articles and 1 abstract which was a RCT
1) There were 3 randomized trials; two were randomized doubleblinded control study and one trial was unblinded with no placebo
2) Two prospective cohort studies
3) One retrospective cohort study
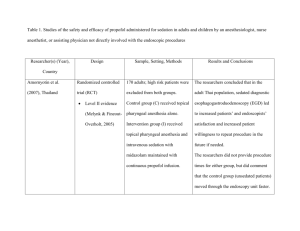
Randomized Controlled Studies
I. Macfie and Harvey; 1977, unblinded randomized trails with 4 groups
A through D
A
77
B
44
C
57
D
41
-Clinda 600mg Iv
1 hr
-I&D
-Curettage
-Primary Closure
-4 day of Abx
Clinda 150mg
-I&D
-Curettage
-Primary Closure
-No antibiotics before or after
-I&D
-Loose packing
-antibiotics
-I&D
-Loose packing
-No antibiotics
Outcome of Macfie and Harvey
A. Total of 219 abscesses studied
B. Group sizes differed significantly because losses to follow up were not recorded
C. Mean healing time varied by 1 day (8.8 to 9.8 days)
D. No recurrence in group A
E. 18% to 25% in other 3 groups
F. Differences were not statistically significant
Conclusion
Antibiotic may marginally reduce the recurrence rate
II. RCT Llera and Levy
A. Randomized, double blinded, placebo-controlled trial over 6 months from 1981 to 1982
B. Inclusion: all adult patients presenting to the ED
C. Exclusion:
– inpatient admission
– Diabetes
– Sickle cell disease
– Any immunosuppressed condition
– Cephalosporin allergy
Llera and Levy Method:
A. All patients had I&D, saline irrigation, loose packing with plain gauze
B. Patient were discharged with a bottle containing cephradine 250 mg or placebo for 7 days
C. Patients returned in 24 to 48 hr for removal of packing and wound check
D. Patient asked to return in 7 days for second wound check
E. Patients who did not come back in 7 days, were followed by a standardized telephone assessment protocol
Llera & Levy Results and Conclusion
A. 81 patients were enrolled, 50(62%) completed the study
B. There were no statistically significant difference between groups with respect to age, sex, race, abscess location or type of follow up
C. 96% in each group showed improvement at the second visit
D. One patient in each group failed treatment
Conclusion
Simple I&D abscess care in patient with normal host defense system heals with or without antibiotic
III. RCT Rajendran et al.
A. Randomized placebo-controlled trial of oral antibiotics after I&D in a high prevalence MRSA population
B. Setting: inner city hospital-based clinic
C. Population: 166 patients with comorbidities such as diabetes, HIV and hepatitis
D. Randomization: Cephalexin or placebo after I&D
Rajendran et al.
Results & Conclusion
A. 110 patients’ wound culture grew S.
aureus ; of these 87 grew
MRSA (52% of study population)
B. There was no difference in clinical resolution between cephalexin
(86%) and placebo groups (93%)
C. Subgroup analysis of patients who grew MRSA did not show any difference in clinical resolution between cephalexin and placebo groups (88% vs. 89% respectively)
Conclusion
Empiric antibiotic use in simple abscesses that have been treated with I&D even in clinical setting of high MRSA prevalence not indicated
IV. Prospective Cohort Studies
A. Lee et al. prospective observational study of children who presented to the ED of a children’s hospital for an abscess and whose culture grew MRSA
B. Patients were identified after culture results were available
C. No exclusion criteria
D. Patients were re-evaluated between 1 to 6 days after initial ED visit and again at 6 to 10 days either by return visit or by a telephone call to primary care provider
69 children with MRSA
5 concordant
(right antibiotic)
2 were admitted
67 patients included
4 were admitted
62 discordant therapy
(MRSA not susceptible to antibiotic given)
58 patients with discordant therapy
21 patients changed to the right therapy
38 patients continued discordant therapy
No significant difference
Lee et al.
Conclusion
• For children without comorbidities and infected sites less than 5cm, treatment with I&D alone in the ED is adequate and adjuvant antibiotic therapy may not be necessary
V. Moran et al.
Prospective Cohort
A. Moran et al. Prospective multicenter study assessed the prevalence of community associated MRSA among adults presenting to university affiliated EDs in 11 US cities
B. 422 patients were enrolled and 320 grew S aureus with 78% being
MRSA
C. Complete treatment information was available on 406 patients
(96% of cohort)
– 267 had I&D + Abx
– 79 had I&D alone
– 39 had Abx alone
– 21 had no treatment
Moran et al.
Results
A. 174 patients grew MRSA and 100 of these patients were given discordant antibiotic therapy
B. Follow up information was available for 248 patients at 2 to 3 weeks follow up (59% cohort)
C. Complete resolution was reported by 238 patients with no significant difference between patients with MRSA or non-MRSA
D. There was no significant difference between patients with MRSA who had concordant or discordant therapy
Moran et al Conclusion
1) MRSA is now the most common identifiable cause of skin and soft tissue infection across the U.S.
2) Concordance between the prescribed antibiotic and in vitro sensitivities of the isolated organism had no influence on the final clinical out-come
3) Thus I&D alone must be sufficient
VI. Retrospective cohort study
A. Payder et al.
Retrospective chart review of Integrated Soft Tissue
Infection Services (ISIS) clinic of SFGH
B. Patients presenting to ISIS clinic for abscess between July 19,
2000 to August 1, 2001were included
C. 441 cultured abscesses with 284 grew MRSA
D. 259 out of 284 (92%) MRSA were treated with discordant antibiotics
E. 4 out of 157 (3%) of methicillin-sensitive S aureus were treated with discordant
Payder et al. Results and conclusion
A. Review of 2 months after treatment showed that 241 out 242
(99.1%) of antibiotic discordant infections had full resolution and
164/166 (98.8%) of antibiotic concordant infection had resolution
B. When adjusted for follow up 92% cure in discordant vs. 99% in concordant groups respectively
C. Conclusion
Addition of antibiotics may be unnecessary after I&D
Limitations
1) None of the studies specifically addressed the issue of abscesses with overlying cellulitis
2) One study excluded patients with comorbidities and immunocompromised conditions
3) None of the studies specifically examined the impact of comorbidities on clinical resolution
Key Points
1) Current data does not support routine antibiotic use after incision and drainage of a simple cutaneous abscess even in high MRSA prevalence area
2)
The need for antibiotic therapy in patients with overlying cellulitis and those with comorbidities or immunocompromised requires further investigation
Abscess Incision and Drainage
Fitch MT et al.
N Engl J Med 2007;357:e20
Clinical Decision Making In Emergency Medicine LLSA
Review 2009
Ehsan Shirazi, M.D.
• Publication: New England Journal of Medicine
• Design: Review article
• Author: Fitch MT et al.
• Site: Department of Emergency Medicine Wake forest University
I. Introduction
A.
Abscesses are common encounter in the ED and
Primary care offices
B. Most common sites are axillae, buttocks, and extremities
C.
Most diagnosed by physical exam based on swelling, redness, tenderness and fluctuance
D. Needle aspiration of a suspected area may help when physical exam is equivocal
E. Bedside ultrasound is helpful in diagnosis and assessment of size, dimension and extension
II. Indications
1) Incision and drainage is the main therapy
2) Most are appropriate for I&D, if they are about 5mm in diameter and in accessible location
III. Contraindications
1) Extremely large or deep abscesses
2) Areas that are difficult to anesthetize
3) Abscesses of the palms, soles, or nasolabial folds require consultation with appropriate surgical specialist
4) Patients at risk for endocarditis such as those with artificial valves may need prophylactic antibiotic prior to procedure
IV. Equipment
A. Universal precautions: gown, glove and face mask with a shield
B. Strict sterile technique may not be required but recommended
C. Items:
1. Skin cleansing agent: Chlorhexidine or povidone iodine
2. Lidocaine for anesthesia
3. Scalpel # 11 or 15
4. Small curved hemostat
5. Normal saline with a syringe and 18-gauge angiocath for irrigation
6.
Wound packing ¼ or ½ in. with or without iodoform
7. Scissors, gauze and tape
V. Preparation
A. Obtain informed consent
B. Discuss the possibilities of pain, bleeding and scar formation
C. Time out; Correct patient, procedure and site
D. Wash hands with soap
E. Clean the area with chlorhexadine or povidone iodine
VI. Anesthesia
A.
Anesthetize by using a 25 or 30 gauge needle and parallel to the surface of the skin
B. Once the entire needle is under skin use gentle pressure to infiltrate the anesthetic
C. Cover the entire surface of the abscess
D. Give additional injections in a local field block pattern
E. IV analgesic or procedure sedation may be needed for some patients
VII. Incision and Drainage Procedure
1) Make an incision directly over the center of the abscess
2) Incision should be along the long axis of the fluid collection
3) Cosmetic results optimized when the incision is made parallel to existing skin-tension lines
4) Incision should be large enough to allow introduction of hemostat to break up loculations and for placement of packing
5) Use a swab or syringe to obtain sample for culture
6) Culture may be useful for the follow up appointment
7) Use a curved hemostats for further blunt dissection to break the loculations
8) Break loculations by a circular motion until the entire cavity has been explored
VIII. Packing
1) Use ¼ or ½ in. packing strips with or without iodoform
2) Start at one quadrant and gradually work your way around the cavity
3) Place sufficient packing to keep the walls separated and allow for further drainage
4) Avoid over packing the wound which may cause ischemia of surrounding tissue and may also prevent further drainage
IX. Aftercare
A. For simple abscess, no antibiotic treatment is required
B. Patients with cellulitis beyond the abscess area and those with comorbidities may benefit from supplemental antibiotic treatment
C. Community acquired MRSA is on the rise with some area up to
74% incidence but no evidence to warrant empiric antibiotic therapy
D. Topical antibiotics are not required
X. Reevaluation
A. Schedule a follow up for 2 to 3 days for removal of packing and reevaluation
B. Instruct patient to return sooner if there is any sign of worsening such as redness, swelling, or development of fever
C. If substantial drainage has continued, repack the wound with fresh material
D. Continued drainage is expected and not an indication for antibiotic use
XI. Complications
A. Developing surrounding cellulitis, lymphangitis, or fever or other signs of worsening may mean the need for repeat I&D and/ or antibiotic treatment
B. Abscess recurrence despite adequate drainage, warrants further investigation o Colonization o Anatomic disorders o Immunologic or infectious disorders
XII. Key Points
1) Use universal precaution and a sterile technique to drain simple abscesses in the ED
2) Large abscesses and those on the palms, soles and nasolabial folds require surgical specialist
3) Incision should be made along the axis of fluid collection and parallel to existing skin tension lines
4) Break the loculations all around the cavity with a curved hemostats
5) loosely but sufficiently pack the entire cavity
6) Empiric antibiotic therapy even in the areas of high prevalence
MRSA not indicated for simple abscesses
Clinical Practice Advisory: Emergency Department
Procedural Sedation With Propofol
Ann Emerg Med 2007;50:182-187
Clinical Decision Making In Emergency Medicine LLSA
Review 2009
Ehsan Shirazi, M.D.
• Publication: Annals of Emergency Medicine
• Design: Evidence based clinical practice advisory
• Authors: James R. Miner, MD and John H. Burton, MD
I. Objective
To provide evidence based recommendations for the use of propofol in the ED deep procedural sedation
II. Introduction
A. Propofol now is the most popular deep sedative in the ED
B. Unlike longer acting agents such as fentanyl and midazolam, propofol is ultrashort acting
C. Literature supports the safety and efficacy of propofol for a variety of ED procedures
III. Indications
• Brief, painful procedures in which deep sedation is indicated i. fractures and dislocation reductions ii. Incision and drainage of abscesses iii. Cardioversion iv. Chest tube placement v. Central line placement
IV. Caution
• Propofol is a suboptimal choice for minimal sedation and/ or moderate sedation in the ED because it is very difficult to stay within this range
• There is not enough evidence to support its safety for longer ED procedures
V. Contraindications
A. Patients with allergy to propofol, eggs, or soy products
B.
Higher relative risk patients
Age: Patients older than 55 years and debilitated patients are more at risk of hypotension
Underlying medical conditions: patients with ASA score of III or IV are at increased risk of propofol induced hypotension
Volume depleted Patients: those patients with dehydration or blood loss are at increased risk for propofol induced hypotension
VI. For High Risk Group
1) Administer lower doses more slowly
2) Optimize patients volume status before giving propofol
VII. Fasting State
A. There is insufficient evidence to support any specific fasting requirements before procedure sedation regardless of agent used
B. Use your judgment regarding:
P atient’s underlying risk factors
Nature and timing of recent oral intake
The urgency of the procedure
Depth and length of required sedation
VIII. Personnel
A. Standard sedation team includes: a ED nurse for patient monitoring and ED physician for performing the procedure
B. Most EDs now require a second ED physician who is not performing the procedure to administer sedation and monitor the patient
C. Propofol package insert states caregivers “not involved in the conduct of the surgical/diagnostic procedure” should administer propofol
IX. Personnel
A. A recent study by sacchetti et al. looked at 1,028 ED sedation encounters where 24% used propofol in which a single physician supervised sedation and performed the procedure
B. Adverse events rate were similar to those for 2-physician sedation
X. Presedation
A. Physician should perform a standard presedation assessment with great attention to potential for air way management
Suction
Airway and resuscitation equipment
Pulse-Ox and cardiac monitoring
End-tidal CO2 monitoring
Supplemental oxygen (its benefit in moderate sedation has been refuted but not in deep sedation)
B. Propofol is not an analgesic
C. It serves a sedative and amnestic agent only
D. Patient may feel pain during the procedure but can not recall later
E. Thus it is recommended that a complete or near complete analgesia be achieved with opiates before propofol is given
Propofol Pharmacology
A. Propofol induces sedation within 30 seconds after injection
B. Half life 1 to 3 minutes and clinical effect resolves within 6 minutes
C. Metabolized by liver and excreted by kidney
D. For ED sedation initial bolus of 1mg/kg followed by 0.5 mg/kg every 2 to 3 minutes to achieve the desired level of sedation
E. This dose is the same for adult and Children
XI. Potential Adverse Effects
A. Similar to other agents; oversedation, hypoxemia, respiratory depression, hypoventilation, airway obstruction, respiratory arrest, hemoynamic instability, nausea, emesis…
B. Respiratory depression (0% to 3.9%)
C. Transient Hypotension (2.2% to 6.5%)
D. Emesis 0% to 0.5%
E. Pain with injection 2% to 20%
XII. Recovery and Discharge
A. Similar to any procedural sedation, patients should be monitored until they have returned to their baseline mental status
B. Since propofol is short acting, no further change in level of consciousness expected after discharge
C. No adverse events after discharge of ED patients treated with propofol has been reported
XIII. Key Points
1) Propofol is indicated for procedures requiring deep sedation such as reductions, I&D, cardioversion, Chest tube
2) Absolute contraindation: allergy to propofol, egg, or soy products
3) Patients who are older than 55 years, are debilitated, or have ASA
III or IV are at increased risk for propofol induced hypotension
4) Volume status should be optimized prior to propofol administration
5) Propofol is not analgesic, therefore it is recommended IV opioids to be given for painful conditions such that complete or nearcomplete analgesia is achieved
6) Dose: Bolus at 1 mg/kg followed by 05 mg/kg every 2 to 3 minutes
Computed Tomography-An Increasing Source of Radiation
Exposure
N Engl J Med 2007;357:2277-84
Clinical Decision Making In Emergency Medicine LLSA
Review 2009
Ehsan Shirazi, M.D.
• Publication: New England Journal Of Medicine
• Design: Review
• Authors: David J. Brenner, Ph.D., and Eric J. Hall, D.Phil, D.Sc.
• Site: Center for Radiological Research, Columbia University
I. Objectives
A. Review CT scanning and its applications
B. Associated radiation doses
C. Cancer risk in adults and children
D. Exposure to radiation as a public health issue
II. Introduction
A. The use of CT scan has increased rapidly in the United States over the past 30 years
B. 62 million CT scans/ year in the U.S.
C. 4 million CT scans/ year in children
D. Total number of CT ordered in 1980 was 3 million
E. There are 26 scanners per 1 million population in the U.S. and 64 in Japan
III. Common Types of CT Scan
A. Half of diagnostic CT in adults are body CTs
B. One third are Head CT
C. 75% are done in hospital settings
D. 25% in a single-specialty practice setting
E. Largest increase for diagnosis is in pediatric population, mostly for appendicitis
F. Largest increase for screening is in adults
IV. Radiation Doses
A. Absorbed dose is the energy absorbed per unit of mass, measured in Grays (Gy)
1 Gy = 1 joule of radiation energy/ kg
B.
Organ dose determines the level of risk to that organ from the radiation
C. Effective dose is the non-homogeneous dose distribution, measured in sieverts (Sv)
An estimate of overall harm to the patient caused by radiation exposure
Allows for rough comparison between different CTs
V. Typical Doses
A. Organ doses from CT scan are much higher than plain radiograph
B. Radiation doses depend on multiple factors
Number of scans
Tube current and scan time (mAs)
Size of patient
Axial scan range
Scan pitch
Tube voltage
VI. Biological Effects
A. Exposure to the X-rays (ionizing radiation) creates free radical known as hydroxyl radicals from water molecules in the body
B. Radicals then damage DNA to cause strand breaks or base damage
C. X-rays also ionize DNA directly
D. Most radiation induced damage is repaired rapidly
E. Misrepair then leads to point mutations, chromosomal translocations and gene fusion which then can lead to induction of cancer
VII. Risks Associated With Low Dose
A. The organ being studied receives a radiation dose of about 15 mSv for adult and 30 mSv in neonates for a single scan
B.
There is a risk of developing radiation induced cancer with doses in this range
VIII. History
A. Most information regarding radiation induced cancer comes from cohort studies of survivors of atomic bomb dropped on Japan in
1945
B. Cohorts are large, studied over decades, covered all age groups and not selected for disease
C. A subcohort of 25,000 survivors received radiation doses less than
50 mSv
D. Subgroups of survivors who received doses 5 to 150 mSv with a mean of 40 mSv had a significant increase risk of cancer
E. An adult who gets a 2 to 3 scans has the same organ dose exposure of 40 mSv
IX. Cohort in Nuclear Study
A. A cohort of 400,000 radiation worker from nuclear industry who were exposed to an average dose of 20 mSv (a single CT in adult)
B. There was a significant association between the radiation dose and mortality from cancer
C. Increase risk of cancer in workers who received doses between 5 to 150 mSv
X. Cancer Risk
A. Individual risk estimates are small
B. But with rapid increase use of CT when applied to a large population, it creates a public health issue
C. From the data on CT use from 1991 through 1996, it has been estimated that 0.4% of all cancers in the U.S. may be due to radiation exposure from CT studies
D. If you adjust it for current CT use, this estimate may be in 1.5 to
2%
XI. How are we doing as physicians?
A. A survey of pediatric radiologists showed that one third of CT studies could be either change to an alternative or not performed at all
B. A survey of radiologists and emergency physicians showed:
75% of the entire group underestimated the radiation dose from CT
53% of radiologist and 91% of ED physicians did not believe that CT scans increased the lifetime risk of cancer
XII. Ways to Reduce Radiation Exposure
A. Reduce CT related dose (related to the scanner)
B. Use alternatives such as ultrasound or MRI when possible
C. Reduce the number of CT scans
Multiple CT scans in blunt trauma
Seizure disorders
Chronic headache
Use as primary tool for diagnosis of appendicitis in children
XIII. Key Points
1) Rapid increase in use of CT scans both as diagnostic and screening tool
2) Compared to plain film, CT involves much higher doses of radiation
3) Organ doses corresponding to a common CT scan can result in an increased risk of cancer in adult and particularly children
4) Increasing exposure to radiation may be a public health issue