Current Controversies in the Perioperative
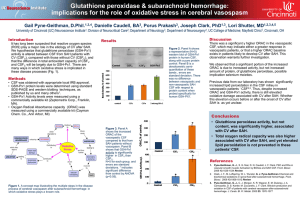
advertisement
Anesthesia for Intracranial Aneurysm Surgery Pekka O. Talke, MD Aneurysms • • • • • • 2-5 % population 30K SAH/yr 2/3 get to hospital 1/3 in hospital severely disabled or dead Unruptured:1-2%/yr rupture Ruptured: 50% rerupture within 6 mo • Urgent, not emergent cases Surgeons • Lawton Anesthetic Goals • • • • • Prevent aneurysm rupture (avoid hypertension) Decrease ICP (surgical exposure, retraction) Maintain CPP (>70 mmHg) Prevent cerebral ischemia from retraction Good operating conditions (NO movement, brain relaxation for exposure) Patients, preop • Symptomatic/asymptomatic • Ruptured (SAH grade, myocardial effects), • • • • • unruptured Possibly intubated Location and size of aneurysm Intracranial mass effect from SAH (increased ICP) Neurologic deficits and symptoms Timing, vasospasm Preop • One IV • Premedicate with up to 2 mg of midazolam if normal mental status. • Remind of potential post op intubation • Adequate fluid loading (5 to 7 ml/kg of LR, angio) Induction • Routine monitors • Propofol or thiopental • Fentanyl 5 ug/kg in divided doses prior to intubation • Muscle relaxant (roc). • Arterial cannula before intubation • Avoid hypertension (propofol) and hypotension (CPP, vasospasm) Induction cont. • • • • • Ceftriaxone 1 gm, 4-10 mg decadron, 1 gm/kg mannitol. Tape eyes with tagaderms (prep solution) Temp probe, foley Additional IV (limited access, 300 cc to liters of blood loss) Compression stockings Positioning • Supine, bump • Long cases, lots of padding (pink and blue foam) • Table turned typically 90 degrees • Head down?, aeroplaning • After draping minimal/no access to face (secure ET well) Maintenance • Oxygen • Propofol infusion (50-200 ug/kg/min) (SSEPs, EEG) • Inhalation agent (<0.25 MAC Isoflurane). Muscle relaxation (vec, panc) • Moderate hyperventilation (ET CO2 30 mmHg) • Euvolemia to 500 cc more (LR) • Moderate hypothermia (34 oC) Burst supression • • • • • • • When requested by surgeon Thiopental 125 mg (5 cc) doses Till 70-80% EEG burst supression Redose as needed Turn fentanyl infusion off Reduce propofol infusion rate Support CPP with phenylephrine infusion Clipping • • • • • • Temporary clips (golden) Permanent clips (silver) Aneurysm manipulation before clipping (bleed) Record clip on/off times Maintain CPP during temporary clipping Start closing, warming and more fluid loading after clipping Toward the end • First indication of end of surgery when clip aneurysm (60 min) • Normalize CO2 once dura closed or earlier if lots of intracranial space • Reduce propofol if possible, and titrate in labetalol Toward the end cont. • Turn propofol infusion off about 10 min before wakeup • Reverse relaxation once Mayfied pins have been removed • Attempt to wakeup patient. Unlikely if more than 1 gm of thiopental given. Recovery • Wake patient up as soon as possible • Extubate if possible • Prevent post op hypertension (bleed). Labetalol • Transport to ICU with monitor and oxygen • Head up position Potential Complications • Delayed awakening from anesthesia • Cerebral ischemia (retraction, temporary clips, vasospasm) • Brain swelling • Intraoperative hemorrhage Aneurysm rupture • Reasonably common • Intubation, pinning, skin insicion, surgical manipulation • Maintain intravascular volume (blood in the room, get help) • Maintain CPP • Adequate anesthesia • Thiopental before temporary clipping Vasospasm • • • • Only if SAH 5-14 days after SAH Leading cause of SAH morbidity (infarct) Maintain CPP at all times (neo infusion, volume) • HHH therapy • Consider CVP measurement What’s new? • Retractor pressure • Temp control • Normotension Surgical Steps • • • • • • • • Mayfield pins (stimulation), head positioning Shaving/prepping/local anesthesia Skin incision (stimulation, blood loss) Scalp off the bone (most stimulation) Burr holes, sawing Removing bone Open dura Surgical approach to aneurysm (microscope, minimal stimulation, retraction) Surgical Steps cont. • • • • • • • Burst supression Temporary clips, permanent clip(s) Close (60 min) Dura (water tight) Bone flap Scalp and skin Dressing, remove pins