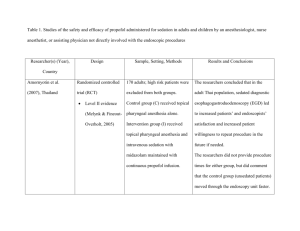
Table 2. Studies of the safety and efficacy of propofol administered
advertisement

Table 2. Studies of the safety and efficacy of propofol administered for sedation in adults during endoscopic procedures by other than anesthesia personnel Researcher(s) (Year), Design Sample, Setting, Methods Results and Conclusions Country Cohen et al. (2003), Prospective descriptive 819 consecutive endoscopic The dose of propofol was negatively United States study examinations in adults under correlated with age and ASA class, Level VI evidence sedation with propofol (63 + 33.5 positively correlated with patient’s (Melynk & Fineout- mg), midazolam (1 + 0.12 mg), weight and duration of examination. No Overholt, 2005) and meperidine (48 + 7.2 mg); 638 supplemental oxygen was given colonoscopies and 181 routinely. Hypotension (> 20 mmHg esophagogastroduodenoscopies decline in either systolic or diastolic (EGDs). blood pressure) developed in 27% adults, and hypoxemia (oxygen saturation < 90%) developed in 9%. All episodes of hypotension and hypoxemia were transient, and no patient required administration of an antagonist or assisted ventilation. The average time for recovery after colonoscopy was 25 minutes and after EGD was 28 minutes. No procedure was terminated because of inadequate sedation/analgesia. The researchers concluded that propofol potentiated by small doses of midazolam and meperidine can be safely administered by specially trained registered nurses and medical assistants under the supervision of a gastroenterologist. All gastroenterologists and registered nurses were ACLS certified. Typically procedures were completed with a gastroenterologist and one endoscopy assistant. Heuss et al. (2003), Prospec-tive descriptive 2,574 adults undergoing 3,475 No major complications occurred Switzerland study endoscopic procedures (upper because of the use of propofol, but Level VI evidence endoscopy, colonoscopy, ERCP, overall decreases in the mean values for (Melynk & Fineout- and endoscopic ultrasonography). oxygen saturation (-2%), arterial pressure Overholt, 2005) Propofol was administered by (-18%), and pulse rate (-10%) were registered nurses under the observed. Hypoxemia probably induced supervision of the by sedation with propofol occurred in gastroenterologist. 43/2,574 patients (1.7%) of patients). In Patients undergoing colonoscopy the other 37 patients, simply arousing the also received meperidine 12.5-25 patient and providing additional oxygen mg IV for analgesia prior to resolved the problem in < 1 minute. In propofol, resulting in a lower dose six (0.3%) of these patients, intervention of propofol being needed. was required consisting of insertion of a nasopharyngeal tube or manual mask ventilation for < 2 minutes. In seven (0.3%) of these patients with persistent bradycardia, atropine was administered. Patients in ASA Classes III and IV had an increased risk of developing or more of these minor adverse events. The researchers concluded that the administration of propofol by registered nurses, with careful monitoring under the supervision of the gastroenterologist, is safe for conscious sedation during endoscopic procedures. Rex, Heuss, Walker, & Retrospective chart 36,743 adults receiving nurse- There were no episodes of endotracheal Rong (2005), United review administered propofol sedation at intubation, death, or neurologic or States three centers—two academic permanent injury. The rate of bag-valve- Level VI evidence Sweden (Melynk & Fineout- hospitals in Indiana, U.S., and mask ventilation was in the order of Overholt, 2005) Sweden and an ambulatory 1/500 to 1/1,000 cases. The authors surgery center in Oregon, U.S. concluded that propofol can be given Patients of ASA > III were safely by appropriately trained nurses excluded. Procedures were limited under the supervision of endoscopists. to EGD and colonoscopies at the U.S. centers, and in addition, some endoscopic ultrasounds and endoscopic retrograde cholangiopancreatography (ERCP) were included at the Swiss center. Saenz-Lopez et al. Prospec-tive descriptive 102 consecutive endoscopies (60 There was no statistically significant (2005), Spain study colonoscopies and 42 EGDs) in difference in mean dose of propofol used Level VI evidence adults. In 27 (26.5%) endoscopies, for EGDs and that used for propofol was administered alone, colonoscopies. The mean dose of (Melynk & Fineout- Overholt, 2005) and in 75 endoscopies (73.5%), propofol when infused alone was 84.8 propofol was combined with mg and in combination with benzodiazepines and/or opiods. benzodiazepines/opiods was 66.9 mg. In All patients were given 4 L/minute colonoscopies, the doses of propofol of supplemental oxygen by nasal required were lower when combined with cannula. midazolam and/or meperidine and in patients over 65 years of age (p = 0.006 and p = 0.001, respectively). Eleven mild to moderate adverse effects were managed by the endoscopist (two vasovagal reactions treated with atropine, a paradoxical reaction to midazolam, and eight episodes of mild desaturation that were corrected by an increase in oxygen flow rate or administration of antidotes. The adults had no memories of the procedure and would be willing to receive the same sedation should the procedure need to be repeated in the future. Although all procedures were completed, tolerance was rated by the endoscopist as excellent/good (83%), fair (5%), and bad/very bad (12%) of EGDs and excellent/good (79%), fair (8%), and bad/very bad (13%) of colonoscopies. The researchers concluded that the administration of propofol by the endoscopist and assistant nurse is an effective and safe method of sedation in adults of both low and high risk as well as elderly patients. The dose of propofol required for an adequate sedation was lower in patients over 65 years and when the medications were combined. The administration of sedation by the endoscopist who performed the procedure or by one assistant nurse is safe and effective. There was no additional person dedicated to monitoring the patient and administering the sedation. The endoscopist was ACLS certified and the nurse was trained in resuscitation skills. Sipe et al. (2002), Blinded RCT 80 ambulatory adults (ASA Class I The mean dose of propofol dose was 218 United States Level II evidence or II) undergoing colonoscopy + 94 mg; mean doses of midazolam and (Melynk & Fineout- alone were randomized to receive meperidine were 4.7 + 1.5 mg and 89.7 + Overholt, 2005) either propofol or midazolam plus 29.1 mg, respectively. Mean time to meperidine by a nurse supervised sedation was faster in the propofol group by an endoscopist. The only task (2.1 versus 7.0 min; p < 0.0001) and of the nurse was to sedate and depth of sedation was greater (4.7 + 0.6 monitor the patient. All versus 3.8 + 1.1, p < 0.0001) compared medications were given by an to the midazolam + meperidine group. induction IV bolus and then Four patients in the midazolam + supplemental IV boluses were meperidine group developed minor titrated to maintain a state of complications (one hypotension and minimal to mild pain while bradycardia, two hypotension alone, and maintaining adequate cardio- one tachycardia) and one patient in the respiratory function. All patients propofol group had oxygen desaturation received 4 L/min supplemental develop during epistaxis. On average, the oxygen. patients receiving propofol recovered faster and were discharged sooner (40.5 versus 71.1 min) (p < 0.0001). Patients who received propofol expressed greater overall mean satisfaction on a 10-point visual analog scale (9.3 versus 8.6, p < .05). At discharge, the propofol group had better scores on tests reflective of learning, memory, working memory span, and mental speed. The researchers concluded that for ambulatory colonoscopy, propofol administered by specially trained nurses supervised by endoscopists has several advantages over midazolam plus meperidine and deserves additional investigation. Tohda et al. (2006), Retrospective chart 27,500 adults undergoing EGD 6.7 % of patients developed oxygen Japan review and/or colonoscopy with nurse- desaturation (< 90%), and 6.2% required Level VI evidence adminstered propofol sedation. supplemental oxygen. Exclusion criteria included Only 121/27,500 (0.62%) developed (Melynk & Fineout- Overholt, 2005) patients with apparent difficult oxygen saturation < 85%, and no patient airways, medication allergies, or required bag-valve-mask ventilation or ASA V status. endotracheal intubation. Supplemental oxygen was not Hypotension (systolic blood pressure < routinely administered. 90 mmHg) was seen in 3.5% of patients; this responded to intravenous saline. Patient satisfaction was high. The authors concluded that nurseadministered propofol sedation under the supervision of an endoscopist was safe. VanNatta & Rex (2006), RCT 200 adults undergoing Patients receiving propofol alone United States Level II evidence colonoscopy randomized to 1 of 4 received higher doses of propofol and (Melynk & Fineout- treatment arms: propofol alone had deeper sedation scores compared Overholt, 2005) titrated to deep sedation or with combination therapy (both p < propofol and fentanyl, propofol 0.001). Patients receiving combination and midalozolam, or propofol, regimens were discharged more quickly midazolam and fentanyl, all three (median 13.0 and 14.7 versus 18.1 titrated to moderate sedation. minutes) than those receiving propofol alone (p < 0.01). There were no differences in vital signs or oxygen saturations among the study arms. There were no significant differences in pain or satisfaction among the study arms in the recovery area. At follow-up telephone calls, patients receiving fentanyl and propofol remembered more of the procedure than those in the other study arms (p < 0.005) and remembered more pain than those receiving propofol alone (p < 0.02). The researchers concluded that combining propofol with midazolam and/or fentanyl allowed a significant reduction in propofol use without an impact on patient satisfaction or postprocedural recovery. Yusoff et al. (2004), Prospective descriptive 500 adults ASA Class I-II There were no major adverse events. Quebec, Canada study undergoing endoscopic ultrasound. Mild hypoxemia (oxygen saturation < Level VI evidence Propofol was administered by the 90%) occurred in 1% of patients that (Melynk & Fineout- endoscopist performing the responded to increasing the flow rate of Overholt, 2005) procedure as an intravenous bolus oxygen per nasal cannula to 4 L/minute, followed by a constant infusion. jaw lift, or temporary cessation of the propofol infusion. The desaturations were caused by upper airway obstruction as a result of propofol-induced hypotonia rather than hypoventilation. There were no episodes of hypotension or bradycardia. The endoscopist rated 92% of procedures as “very smooth” or “smooth” and regarded administration of propofol as easy. All patients reported they would prefer the same sedation if the procedure were repeated. The endoscopist was ACLS certified and the nurses were BCLS certified. The authors concluded that although safe, the use of propofol was more stressful and labor intensive for the endoscopist compared with conventional sedation with midazolam and meperidine. Constant attention was required from beginning to end of the infusion and episodes of propofol-induced oxygen desaturation, even when mild, engendered greater anxiety for the entire endoscopy team. Because of the absence of a dedicated person to monitor the patient, relatively conservative loading and infusion doses of propofol were used resulting in undersedation with frequent gagging during intubation and coughing during the procedure. Also, there were more procedure interruptions. Therefore, the researchers concluded given the inherent peculiarities of propofol-induced sedation, it may be best to reserve its use for patients in whom standard sedation is expected to be inadequate.