RSI Case Discussion Draft
advertisement

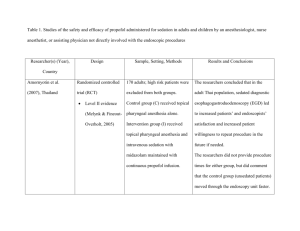
RSI Case Discussion (Below case is discussed assuming you’ve completed the recommended readings – if you haven’t yet, please do so prior to continuing) Part I SW is an 80 kilogram 61 year old female seen at an outside facility for new onset respiratory distress. PMH includes obstructive sleep apnea, hypertension, cigarettes 40/pack year. Home meds are losartan, metoprolol, hydrochlorothiazide. Three days ago SW began experiencing wheezing, coughing, and shortness of breath. This morning she presented to an outside clinic hypoxemic, tachypneic and uncomfortable appearing. She received nebulized ipratropium and albuterol with no effect and was transported by medics from clinic to the ER. On arrival, SW was receiving O2 by nonrebreather at 15L/min,wheezing heavily with following vital signs (as of 1530): BP 159/89, HR 72, RR 36, SpO2 75, T 37.9. At 1545 SW was given iv methylprednisolone 125mg. At 1600 she demonstrated altered mental status with combativeness. She aggressively refused medical care in her altered status, and at 1610 40mg of ketamine was given. Updated vitals (as of 1615) :BP 179/96 , HR 98, RR 27, SpO2 73, T 38. Pt continued to be combative, refusing O2, and the decision was made to intubate her. Questions for Discussion: Discuss appropriate preparation for rapid sequence intubation - What pharmacologic agents would you want to have on hand and why for SW? What additional information would we want prior to making medication recommendations? Discuss dosing and rationale for ketamine. Case Discussion Part 1 – What should we be thinking? SW meets at least 2 of the 3 most commonly cited indications for RSI: 1) Protect the Airway, as we might see in severe drug/alcohol overdoses. 2) Maintain ventilation and oxygenation – If a patient’s SaO2 drops to less than 90% for prolonged periods of time while on high flow oxygen or if the patient is having a difficult time breathing off C02. (PaCo2 is>55, for example.) 3) Expected decline in clinical status - expected progression of current symptoms, altered mental status, or combativeness. Her smoking and sleep apnea history increase risk for developing both hypoxemic and obstructive respiratory failure, but it is her acute presentation that should put us on RSI alert. With 3 days of wheezing, persistent SpO2 levels in the 70s in spite of oxygen 15L/min via nonbreather, and combative altered mental status, we need to prepare for imminent intubation. Seven major steps, commonly referred to as the “seven Ps” are involved in RSI: 1) Preparation 2) Preoxygenation 3) Pretreatment / Induction 4) Paralysis 5) Patient Placement/Positioning 6) Placement of Tube in Trachea 7) Postintubation Management For SW, Preparation begins once the charge nurse finds out that SW is coming in with significant respiratory distress. For ED Pharmacists, Preparation includes the process of gathering SW’s pertinent information required for sedative, analgesic, reversal agents, and paralytic selection / dosing. As much as time allows, the ED Pharmacist reviews SW’s chart and talks with family members – in addition to the above noted medical history, we see that SW’s current electrolytes are all within normal limits including a potassium of 4.2, good renal function with Cockroft-Gault GFR>90 ml/min. SW is negative for burn injury, intracranial processes or trauma. We pay particular attention to her vital signs and weight, we find that she has no known medication allergies and no known food allergies. In addition to preparing RSI agent options the ED Pharmacist also makes sure that a “crash cart” with ACLS medications and resuscitation fluids is available in case SW’s clinical situation becomes more critical. Meanwhile, the rest of the ED team has contacted respiratory therapy and made sure that the bag-valve-mask (“ambu bag”) and intubation equipment are available as well as pulse oximetry, cardiac monitoring, and end tidal CO2. Also during Preparation ED providers assess SW’s potential for “difficult airway” or “difficult intubation.” Factors that can indicate a difficult airway include patients with large beards, obesity, lack of teeth, old age, and patients who snore – SW is negative for this so we wouldn’t expect a difficult intubation but the ED Pharmacist, having assisted with the selection of appropriate agents, would use this information to help calculate necessary redosing of sedatives, paralytics or analgesics. Physicians, Medical Assistants, Respiratory Therapists and Nurses are largely involved in these latter Preparation processes, but the ED Pharmacist must take part in these discussions in order to anticipate appropriate medication selection, doses, and the potential need for additional emergency medications. Once the specific agents/doses have been decided upon, the final step of Preparation is to pre-draw all of the medications into labeled syringes for easy and quick administration during intubation. Meds we want to have on hand fall into the broad categories of Pretreatment meds (discussed separately), analgesics (almost always Fentanyl), sedatives (Midazolam, Etomidate, Ketamine, Propofol) and neuromuscular blockers (Succinylcholine, Rocuronium, Vecuronium). SW received methylprednisolone to decrease inflammation, improve oxygenation and hopefully stave off intubation. When this failed and SW’s mental status declined, Ketamine was given. Ketamine was probably chosen because it has both analgesic and dissociative properties and is also a drug often used in RSI. Doses of ketamine used in RSI are 1.5-2mg/kg pushed, so SW’s anticipated full RSI dose would have been 120-160mg Ketamine; the dose given here reflects 0.5mg/kg and probably represents either a sub-dissociative attempt at pain control or an attempt to mildly sedate the patient and either assess the true need for RSI or give the patient the best chance at Preoxygenation, the second step of RSI. Preoxygenation is attempted to increase SW’s SpO2 by having her breathe 100% oxygen through nasal cannula or non-rebreather. We would like SW to take deep breathes for at least 2 to 3 minutes, but preferably 5 minutes. This would help SW store oxygen so that once RSI is begun her SpO2 will remain elevated long enough for the endotracheal tube to be placed. If preoxygenated appropriately, the average 70 kg adult will be able to maintain O2 saturations above 90% for 7-8 minutes before steeply dropping, although this variable is affected by multiple factors including comorbidities, age, and obesity: Based on SW’s weight and degree of illness we would expect her to maintain her saturations for 5-6 minutes if appropriately preoxygenated. Unfortunately, SW’s altered mental status and combativeness preclude this step. We might anticipate SW’s SpO2 to drop much sooner than expected, requiring a pause in RSI during which a bag-valve mask is used for respirations. These pauses would be required to keep SW oxygenated, but they can prolong RSI to the point of requiring additional doses of induction medications. SW being at risk for prolonged RSI, we should anticipate a need for sedative/analgesia/paralytic redosing. Part II Labs drawn at 1620 show: Na 141, K 4.2, Cl 96, CO2 35, Glucose 125, BUN 14, SrCr 0.7 At 1702 SBP/DBP was 179/96, HR 98. ED Team has decided upon propofol and succinylcholine. At 1708, 125mg of propofol was given by iv push. Succinylcholine 120mg was pushed at 1710. Intubation went without incident, propofol infusion began at 1720 at 20mcg/kg/min. At 1711 SBP/DBP 144/76, HR 89. At 1730 SBP/DBP was 89/48, HR 79. Questions for discussion: Discuss the selections for sedation and neuromuscular blockade and what alternatives might have been considered. What would you have recommended for analgesia? Discuss SW’s hemodynamics. Analgesia would normally take place during the third step, Pretreatment, minutes prior to tube placement. Pretreatment involves administering medications for the purpose of decreasing the body’s natural response to intubation. Sympathetic and parasympathetic stimulations can release catecholamine during RSI resulting in tachycardia and transiently elevated MAPs while intubation itself can stimulate upper airway reflexes which in turn can increase intracranial pressure (ICP). The acronym LOAD (Lidocaine, Opioids, Atropine, Defasciculation) has described pretreatment, although we opted to avoid the majority of these agents for SW as they have largely fallen out of common use. Lidocaine (pretreatment dose is 1.5 mg/kg iv pushed before intubation) blunts the body’s reflexive increase in ICP. The ideal candidate for lidocaine pretreatment would have risk factors for ICP elevation such as closed head injury or traumatic brain injury. We have no reason to suspect elevated ICP for SW we choose not to use lidocaine. Lidocaine can also be dangerous in patients with bradycardia, heart block, hepatic failure or patients taking dofetilide, moa inhibitors or amiodarone. Atropine has historically been used during pretreatment to blunt the possible bradycardia effect of succinylcholine, but current standard of practice in adults is to avoid pretreatment with atropine in favor of having it available in case significant bradycardia does occur after induction. Atropine is more often used in pediatric patients at a dose of 0.01 mg/kg, with a minimum dose of 0.1 mg. SW did not receive atropine and her heart rate tolerated the procedure well. Defasciculating agents are a class of Pretreatment meds given on occasion to blunt the myoconal fasciculations caused by succinylcholine. These agents are rarely used in the ED – note that no defasciculating agents were used in SW. Had she received defasciculation, vecuronium is the most commonly used agent, typically at doses of 0.01 mg/kg 3 minutes prior to administration of succinylcholine. Of all the Pretreatment medications, Opioids are the most commonly given agents and due to rapid onset of action and minimal histamine release Fentanyl is the opioid of choice. For SW fentanyl would be a good recommendation to provide analgesia and to help decrease the catecholamine flood that can occur during intubation. Although fentanyl has minimal cardiovascular effect, opiates are often avoided in patients presenting with decompensated shock; while analgesia remains an important component of patient care, hemodynamic instability warrants cautious dosing . It’s worth noting that SW’s agitated state may be a clue to excessive catecholamine release – patients experiencing high catecholamine states (withdrawal syndrome, severe pain) pre-intubation may experience abrupt drops in blood pressure when catecholamine blunting drugs like sedatives and analgesics are given during the intubation process. SW’s agitation should serve as a warning that her post-intubation course is going to be hemodynamically challenging. Fentanyl is generally dosed pretreatment at 1-3 mcg/kg iv push. . After the premedications are selected and given, the fourth Step is Paralysis with Induction. SW is treated with Propofol due to rapid onset of action and rapid elimination. Propofol decreases cerebral oxygen consumption and ICP, and may be an attractive option in patients with elevated ICP, but is also known to reduce preload, afterload, and cardiac contractility. A 10-20 mmHg drop in systolic blood pressure can be anticipated with propofol induction doses, making it a less attractive option in hemodynamically fragile patients, and we see that SW responds with an even more dramatic drop postintubation than we might expect from propofol alone. Propofol can induce bronchodilation, making it a reasonable option in patients with reactive airway disease, so SW might benefit from propofol’s bronchodilation properties, but the first post-intubation blood pressure should raise concern about propofol’s cardiac properties. SW’s excessive drop in blood pressure should also make us suspect that additional, non-pharmacologic processes might be at work putting SW at increased risk of Post-Intubation Hypotension (PIH). 125mg of propofol is an appropriate dose for SW, (induction range 1.5-2.0mg/kg), and pharmacologic effect is seen within 1-2 minutes – it’s important to verify that sedation is induced when paralytics are used, since paralysis without sedation is inhumane and can induce life-long trauma. Propofol induction lasts 5-10 minutes after which either maintenance sedation should be started or, if intubation is still in process, redosing should be prepared. Propofol is delivered in a soy-based fat emulsion so SW and family confirm for us that there are no allergies to medications or food including sensitivities to soy. Sensitivies to eggs and peanuts are often ruled out as well, although evidence for this cross-sensitivity is limited to a small number of case reports and is controversial; use of propofol in patients with peanut or egg allergies should be considered on a case-by-case basis. Midazolam could have been considered for SW due to its amnestic, anxiolytic, hypnotic and sedative effects as well as its potential to lower blood pressure. Midazolam is the benzodiazepine of choice as its high lipophilicity creates a more rapid onset in the high lipid content of the brain. Midazolam is much more likely to be used as a post-intubation sedative than as an induction sedative due to the large doses required for induction: For appropriate induction, doses of 0.2-0.3mg/kg (>20mg in an average patient) are required and can take several minutes for onset, longer than other more attractive induction options. Etomidate is a commonly used sedative in RSI induction (not maintenance) and would be suitable for SW - a typical dose of 0.2 to 0.3 mg/kg will take effect in 30 seconds and last 5-10 minutes. Unlike propofol or midazolam, etomidate is not likely to lower blood pressure, and unlike ketamine it is not likely to raise blood pressure. Furthermore, etomidate can attenuate elevated ICP making it a very attractive agent if we were concerned about ICP in SW. Of theoretical concern, etomidate has been shown to be associated with adrenal suppression even in one-dose use. The importance of this is unclear with studies failing to show clinical significance, but if we were concerned about sepsis or SIRS in SW we might consider alternative agents. We see that SW already received a subdissociative dose of Ketamine, a phencyclidine derivative with a rapid onset of action providing analgesia, preserved respiratory stimulation and dose-related amnesia. As opposed to propofol, ketamine is associated with an increase in systolic blood pressure , so it is a reasonable option in patients with hypotension. SW doesn’t present with hypotension, although ketamine may be beneficial in SW’s reactive airway disease since it directly relaxes bronchial smooth muscle and potentiates the bronchodilatory effects of epinephrine. In patients with no autonomic control or catecholamine depletion ketamine may act as a negative inotrope/chronotrope. SW’s sudden pre-intubation agitation is suggestive of a catecholamine surge, which may subsequently lead to catecholamine depletion at which point ketamine might begin to exert negative inotrope effects. However, as catecholamines become depleted or blunted, blood pressures drop at which point ketamine might look like an attractive option – this paradox vividly demonstrates that post intubation hypotension can be extremely complex and multifactorial; agent selection should be made on a case by case basis taking into consideration the cause of hypotension, patient dynamics and the potential risk/benefits for each individual situation. In SW the sedative agent was given, as it always should be, before the neuromuscular blocker. Neuromuscular Blocking Agents (NMBAs) possess neither analgesic nor sedative properties, so the inappropriately sedated patient would be fully paralyzed while retaining complete awareness- an inhumane and nightmarish picture. Neuromuscular blocking agents (NMBAs) mimic the action of acetylcholine in order to block neuromuscular transmission and SW has received succinylcholine for paralysis. Succinylcholine is frequently chosen, as it is in SW, because it produces neuromuscular blockade rapidly has a brief duration; it so closely mimics the action of acetylcholine that it depolarizes the postsynaptic membrane with resultant muscle fasciculation just prior to full paralysis. As the muscles fasciculate they release potassium, on average increasing the serum potassium level by 0.5 mEq/L. In patients with a history of hyperkalemia, potassium levels may increase dramatically, as much as 5-10 mEq/L, and in patients with burn injury, trauma, or severe infection, the potassium increase may take place well after the exposure. All of this means that while succinylcholine is the gold standard for RSI paralytics, utilized in more than 80% of RSI cases, it should not be used in patients who are either hyperkalemic or at increased risk of hyperkalemia (trauma,burn, renal failure). A history of malignant hyperthermia is a contraindication to succinylcholine use. Succinylcholine can also preciptate bradycardia by stimulating muscarinic receptors. Happily SW has no history of malignant hyperthermia per family, has a good heart rate and reasonable potassium levels so succinylcholine is a good option for SW at an appropriate dose of 1.5 mg/kg iv push. If we were unable to obtain any history for SW or uncertain about any of her risk factors, a non-depolarizing neuromuscular blocker with a relatively short/intermediate duration of action like rocuronium (0.6-1.2 mg/kg) or vecuronium (0.1-0.25mg/kg) would have been appropriate. Nondepolarizing neuromuscular blockers are much less likely to cause hyperkalemia or malignant hypertension, but they last significantly longer than succinylcholine and it can take longer for onset of action. Step 5 is Protection/Positioning followed by Step 6, Placement. SW’s intubation went well and without incident, however if the intubation was difficult, generally determined by difficulty placing the tube, Placement would have been stopped to provide the patient with further oxygen. Re-dosing of the sedative and paralytic may have also been necessary given their short durations of action, and the ED pharmacist should always have an understanding of what dosages would be appropriate for redosing and what factors might predict an extended or complex procedure. At this point, our primary concern should be SW’s decreasing blood pressure in the post-intubation stage. Part III Propofol drip was turned off at 1730, and by 1735 SW began to arouse. Midazolam was given as a bolus for sedation and a midazolam infusion was intiated at 1800. Despite turning off the propofol drip at 1730, her BP remains a concern: 1805 1831 20:06 20:15 20:30 20:45 21:00 22:00 SBP 49 134 100 102 107 105 115 108 DBP 25 48 43 30 32 32 36 30 HR 66 45 56 54 59 57 60 73 62 55 59 55 63 MAP SW was started on epinephrine infusion at 1830 and shortly afterward dobutamine was initiated. She was transferred to the ICU for further management of respiratory failure and shock. Case Discussion: Discuss SW’s post intubation care. Discuss the use of propofol and midazolam in this patient – what other alternatives for sedation are available and what are the benefits/drawbacks of these alternatives? Step 7, Postintubation Management, begins promptly after intubation and includes the provision of ongoing analgesia and sedation for intubated patients. Pharmacists have been shown to improve the quality of postintubation sedation by reducing the amount of time it takes to continue sedatives after intubation. This becomes extremely important when intermediate acting paralytics (rocuronium, vecuronium most often) are used – the longer the duration of paralysis, the more important it becomes to keep patients continuously sedated with no interruption between the induction and maintenance phase. For example, note that SW received her initial propofol push at 1708, and succinylcholine was given at 1710. The initial propofol push will probably last 5-10 minutes, while the succinylcholine will last 5-8 minutes; we want to make sure that SW doesn’t begin to wake up before the succinylcholine is eliminated. Had rocuronium been used instead of succinylcholine, the paralytic duration of action would extend beyond the duration of initial sedation coverage making it even more important to begin maintenance sedation promptly. For SW, her postintubation sedation infusion began 12 minutes after the initial propofol push and 10 minutes after the paralytic was given - this may be within reason for succinylcholine since the initial dose of propofol would have outlasted the duration of succinylcholine, but we should still be aiming for a more rapid transition. There is evidence that patients receiving rocuronium receive less post-intubation sedation than patients receiving succinylcholine, presumably because it is more difficult to determine specific need for sedation in a patient with extended paralysis. Postintubation sedation is most often performed with a continuous infusion of either propofol or midazolam and in SW the first agent chosen is propofol at 20mcg/kg/min. Starting maintenance doses for propofol infusions range from 5 to 20 mcg/kg/min and can be titrated up to 70 mcg/kg/min using blood pressures and sedation level as titration guides. Recall that following the initial propofol induction push, SW’s systolic dropped by 35 points – this might have suggested to us that SW’s maintenance propofol dose should be chosen with caution, perhaps starting at 10mcg/kg/min. It’s also possible, given the extent of the decrease, that SW’s PIH is a result of non-pharmacologic factors and would have occurred regardless of agent selection and dosing. This may also explain SW’s persistent PIH long after propofol had been turned off. Note that within 5 minutes of turning off the propofol SW begins to wake up so midazolam was initiated as a bolus to maintain sedation. Midazolam is not an unusual choice since it is less cardio depressant than propofol, is easy to bolus while drips are being prepared, and is readily available in most Emergency Departments. Unfortunately, midazolam can also cause hypotension, but it’s a reasonable option for SW at this point. Ketamine given as a drip may also be given here in the hopes of increasing blood pressures, but if ketamine is selected it should be done with caution; in the catecholamine depleted patient ketamine loses much of its effect on blood pressure while keeping its potential effect as a negative cardiac inotrope. More concerning, ketamine has a longer half life than propofol so ketamine, when given for post intubation maintenance, should be initiated at low doses with a close eye on pressures. Dexmedetomidine is an option more frequently seen in the ICU than the ER but may be an option in patients whose blood pressure is too low for either propofol or midazolam. Doses of 0.2 to 0.7 mcg/kg/hr are used to maintain sedation. Analgesics are required in patients who remain intubated and can often assist in balancing and reducing the overall dose of sedatives required. Fentanyl boluses or drips are typically started at 50 100mcg/hr and titrated to response. At 1805, more that half an hour after propofol was discontinued, SW’s PIH had continued with a systolic of 49. It cannot at this point be assumed that PIH was a result of simple propofol dosing and pressors are initiated to keep a MAP above 60. Postintubation hypotension (PIH) is a worrisome complication of intubation, associated with increased inhospital mortality. Heffner et al. demonstrated a presence of PIH in 25% of previously normotensive patients. As pharmacists we often associate PIH with sedative agents, as the medications we use to relax patients during ETI reduce catecholamines, leading to arterial and venous dilatation. The true cause of PIH is multifactorial and may include reaction to medication, induction-associated sympatholysis , effects of positive-pressure ventilation, or it may be a late sign of cardiovascular insufficiency that occurs once compensatory mechanisms to maintain normal perfusion pressure are either overwhelmed or exhausted. Systolic blood pressure < 70mmHg have been reported in 10% of intubations in critically ill patients (Griesdale), while another study reported a 2% risk of cardiopulmonary arrest during endotracheal intubation associated with PIH. (Mort TC. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: A justification for incorporating the ASA guidelines in the remote location. J Clin Anesth 2004;16:508-16) Risk factors noted to contribute to PIH include age (older patients at higher risk), comorbidity, patients on B-blocker therapy, and patients with lower mean SBP immediately prior to intubation. It has been suggested that in patients at high risk for PIH, and conditions permitting, excessive loss of vascular tone might be reduced or prevented by inducing intubation with multiple small doses or increments of intravenous sedatives every 5-10 minutes (1-2 mg midaz or 0.3mg/kg lean body mass propofol) rather than bolusing a single large dose of sedative. In specific patients it may be possible to attempt endotracheal intubation using verbal commands and local anesthesia in the absence of sedatives. Other recommendations proposed to reduce the incidence of PIH include beginning volume resuscitation – wide open NS – in all but evidently hypervolemic patients expectantly during ETI, especially when patients are very catecholamine driven before ETI and ensuring that a pure vasoconstrictor, for example, phenylephrine, is rapidly available in case the rate of fluid resuscitation is insufficient to refill the system until more vascular tone returns with awakening. Sedative Agent Induction Comparison Chart Drug Etomidate (Amidate) RSI Dose 0.2-0.3 mg/kg Time to Effect 30 sec Length of Effect 10 min Propofol(Diprivan) 1.5-2.5 (2) mg/kg 1 min 5-10 min Ketamine (Ketalar) 1-2 (1.5) mg/kg 1 min 5-10 min Midazolam (Versed) 0.03-0.04 mg/kg Typically underdosed 0.2-0.3 mg/kg may be more appropriate 1-2 min 15-20 min Dexmedetomidine (Precedex) 1 mcg/kg 5-10 min 60-120 min Neuromuscular Blocker Comparison Chart Drug RSI Dose Time to Effect Length of Effect Succinylcholine (Anectine) Depolarizing NMB 1.5 mg/kg 1 min 3-5 min Rocuronium (Zemuron) Nondpolarizing NMB 0.6-1.2 (1.0) mg/kg 1-1.5 30-110 min Vecuronium Nondpolarizing NMB 0.1-0.25 (0.15) mg/kg 1-3 min 30-120 min Cisatracurium (Nimbex) Nondpolarizing NMB 0.1-0.2 mg/kg 2-3 min 20-90 min Pancuronium Nondpolarizing NMB 0.1 mg/kg 2-5 min 40-100 min