Performance Improvement: Making It Simple for
advertisement

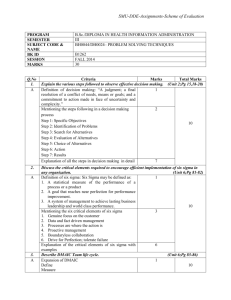
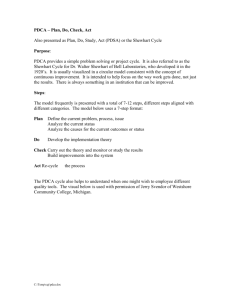
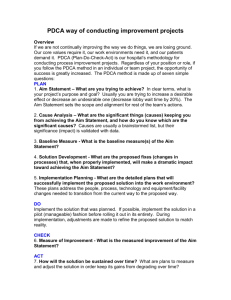
Performance Improvement: Making It Simple for the Creative (Busy) Minds Norma A. Atienza, BSN, MPA, RN, CIC, CPHQ October 26, 2011 Quality / Performance Improvement Definitions: A planned, systematic, approach to monitor, analyze and improve performance, thereby continually improving the quality of patient care and services provided and the likelihood of desired patient outcomes. The continuous study and adaptation of a healthcare organization’s functions and processes to increase the probability to better meet the needs of individuals and other users of services. Quality / Performance Improvement Process • PI Projects are identified / approved by the governing body as initiatives that are important to support the mission and the strategic goals of the organization • Projects are also identified based on high volume, high risk and those that affect patient care that potentially will have negative outcomes. • Infection Control – looking at processes and outcomes that supports the goals of the practice aligning to the strategic goals of the institution. Why Performance Improvement? The quest for Quality has become relentless especially with the advent of health care reform Quality initiatives have become more prominent not only with government initiatives that set specific benchmarks to improve patient care but also among other health care insurers. Common PI Methodologies or Approaches: Shewart Cycle / PDCA or PDSA Cycle PDCA was developed by Walter Shewhart in the 1920s and Edwards Deming adapted the process and called it PDSA Cycle – Plan • Plan change • Study a process by collecting necessary data • Evaluate the results • Formulate a plan for improvement • Set goals and target • Determine methods for reaching goals – Do • Implement the plan (trial, house-wide) • Educate / train – Check or Study • Gather data and evaluates results of the change • Determine success of action taken • Modifications needed – Act • Implement the plan changes • Not successful, abandon the plan and rework the cycle FOCUS - PDCA Model Originated with the Hospital Corporation of America now HCA Healthcare. It assumes that a PI or a QI process is already in place to improve. • F = Find a process to improve – define the process, identify the process – who will benefit from the improvement – how the process fits w/in the org priorities • O = Organize a team that knows the process – people knowledgeable about and involved in the process – manageable team size, appropriate members – method to document team progress (WWW) • C = Clarify current knowledge of the process – gather and review current knowledge – analyze to distinguish between expected and actual performance • U = Understand variable and causes of variation – Plan and implement data collection – Measure using appropriate indicators • Select = the process improvement – Identify action to improve Other Approaches to Performance Improvement • Change Acceleration Process (CAP) – A process that proactively plans for change acceptance for successful implementation – Streamlines “traditional QI approaches – Requires top leadership support to succeed • Work-Out – Promotes rapid problem solving via involvement and accountability – Flowchart, cost/benefit of solutions – Test period or pilot • Lean – Focused on eliminating waste through detailed analysis of workflow Six Sigma Strategy • Was a strategy developed by Motorola in the mid1980s and implemented successfully in GE and Allied Signal (manufacturing) as a way to reduce common cause variation and error rates. • Driven by statistical analysis of data to identify causes of unwanted variation and defects DPMO Quality Yield COQ/COPQ (% quality standards achieved) Poor Cost as % of total 1δ & 2δ Defects / million opportunities 700,000/308,537 3δ (non-competitive) 66,807 93.3% 25-40% 4δ 6210 99.4% 15-25% 5δ 233 99.98% 5-15% 6δ 3.4 99.999% <1% Sigma Value (world Class Adapted from: Caldwell, Brexler, Gillem. Lean-Six Sigma for Healthcare High The DMAIC Approach D: Define • • • • Define the problem Set the goals Identify the customers Who are your team members M: Measure • How is the process performed • Identify the metrics • What data will be collected • Methodology in collecting the data The DMAIC Approach A: Analyze • Review data, what have the PI tools revealed (fishbone, flowchart, etc.) • Identify or diagnose root cause • What is the data telling us I: Improve • Improve the process • Identify actions needed to achieve the performance goal • Apply WWW process as needed • Implement actions for improvement • Review and compare old and new process, what was changed The DMAIC Approach C: Control • In control only when goal is reached – then maintain and monitor the improvements Review data, what have the PI tools revealed (fishbone) • If not, go back to data analysis. Review improvement processes in-placed, are they effective? • Make changes as needed. Metrics • Outcome • Process • Person Centered • Structure Developing Goals S – specific M – measurable A – attainable R – relevant T – time based C – clearly understood A – agreed upon R – re-negotiated Judy L’s Examples: 1. To decrease HA CAUTI by 10% by the end of FY2012 from that of 2011. 2. By June 30, 2012, improve Core Measure aggregate perfect care score to 95%. 3. Reduce department expenses by maintaining no more than 1.8% (of total Salaries) in overtime expenses each month as reported in Visionware. Review of Common Graphs and Charts Line Graph or Run Chart: provides a running record of a process overtime Saint Clare's Hospitals Falls Data - July 2010 to April 2011 per 1000 Patient Days 4.50 4.02 4.00 3.76 3.50 3.10 2.95 Goal Ave = 2.70 2.71 2.49 2.50 2.29 2.00 1.48 1.50 1.45 1.00 0.50 Month Apr Mar Feb Jan Dec Nov Oct Sep Aug 0.00 Jul Fall Rate 3.00 2.66 Line Graph Saint Clare's Hospital Mortality '10 4.50 RRT '10 4.22 4.00 3.50 3.30 3.00 2.50 2.00 1.85 1.65 1.50 2.27 2.09 1.10 1.00 2.03 1.80 1.44 1.17 0.98 1.11 1.43 1.25 0.50 0.00 Mortality rate continues to decrease in 2010 except for the couple of months. Again if RRT is decreased, mortality rate increased Jan Feb Mar Apr May Jun Jul Aug Pie Chart or Circle Graph: used to display parts of a whole (proportional relationships) Saint Clare's Hospital Site of CVAD Insertions January to Decem ber 2010 26% 31% Subclavian Femoral 5% IJ Upper arm (PICCs) 38% Control Chart: a display of normal variations and “out of control” variations over time Denville TAT 80 1 70 Individual Value 60 UCL=53.46 50 40 _ X=30.34 30 20 10 LCL=7.23 0 3 5 7 1 3 7 9 1 5 8 1 3 7 9 1 5 7 1 3 5 1 3 7 9 1 1/ 1/ 1 / 1/1 1/1 1 /1 1/1 1/2 1/2 1 /2 2 / 2/ 2/ 2/ 2/1 2/1 2 /1 2/2 2/2 2/2 3/ 3 / 3/ 3/ 3 /1 date1 Bar Chart: comparisons between different groups Saint Clare's Hospital Handwashing Compliance Hospital-Wide Discipline Specific 100 80 60 40 20 0 Phys Nsg NAs APN CM/S Anc. PT/OT Trans Rad Resp Env. Phleb Other W Tech /ST port Techs 2009 73.5 96 91 78.6 69.6 88 77.8 80.4 67.7 31.9 66 42.1 83.9 2010 98.4 95 92.9 75 78.9 100 92.5 96.3 73.1 60 92.2 56.1 94 2009 2010 Pareto: offers a comparison of causes of problems in a process and rank-order (prioritizes). Determine where to focus improvement efforts. 250 100 200 80 150 60 100 40 50 20 0 Comments P o e rF w o Po o rF we Count Percent Cum % 22 rm no rm t nt se e r p M ng ssi i m D 132 52.0 52.0 n e/d am Po e /tim e t a rF we m or s mi g sin P 95 37.4 89.4 MD n e am Fo er w o rm ng issi m 13 5.1 94.5 d e /tim e t a 11 4.3 98.8 O er th 3 1.2 100.0 0 Percent Count Pareto Chart of Critical Values PowerForm Audit Realize that change is not always a process improvement. Sometimes it’s a process of invention! Wendy Kopp Founder of Teach for America ? Questions