Neisseria - Pathology
advertisement

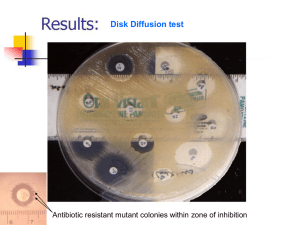
EPID 525 Lecture 2 Manual and automated methods for organism identification Microscopy • Magnification – enhancement of size using ocular and objective lenses. • Ocular: eyepiece (10X) • Objective: 4X – 100X – allows for visualization of bacteria, fungi, and parasites, not viruses • Resolution – ability to distinguish two objects as distinct – resolving power is closest distance between two objects – immersion oil is added when using 100X objective to prevent light scatter • Contrast – use stains to enhance visualization; allow organism to stand out from background Staining techniques • make slide by smear, drop, or cytocentrifuge • dry, then fix by heat (flame, 10 min at 60ºC) or fix by methanol (95% 1min) • Gram stain – – – – Crystal violet: primary stain Gram’s iodine: mordant/fixative Acetone-ethanol: decolorizer Safranin: counterstain http://www.sp.uconn.edu/~terry/229sp02/lectures/Lect2.html Neisseria gonorrhea - Gram stain http://www.cdc.gov/STD/LabGuidelines/default.htm Wound specimen - Gram stain http://www.healthsci.utas.edu.au/hls/teaching/micro/mma.html Oral specimen - Gram stain http://www.healthsci.utas.edu.au/hls/teaching/micro/mma.html Sputum specimen Gram stain—Streptococcus pneumoniae http://www.healthsci.utas.edu.au/hls/teaching/micro/mma.html Sputum specimen Gram stain—mixed oral flora http://www.healthsci.utas.edu.au/hls/teaching/micro/mma.html Sputum—cystic fibrosis patient, encapsulated gram negative rods http://www.healthsci.utas.edu.au/hls/teaching/micro/mma.html Staining techniques • Acid-fast stains – for staining of organisms with high degree of fatty (mycolic) acids—waxy – render the cells resistant to decolorization: “acid-fast” – Mycobacterium sp., Nocardia sp., Cryptosporidium sp. are acid-fast – Procedure • • • • Ziehl-Neelsen: heat drives in primary stain (carbolfuchsin) Kinyoun: higher conc. of phenol does not require heat Decolorize with acid-alcohol Counterstain with methylene blue or malachite green A Gram stain (left) of the abscess shows thin, gram positive rods in chains. An acid fast stain (right) was also positive. http://pathhsw5m54.ucsf.edu/overview/bacteria3.html Sputum specimen—Acid fast stain http://www.healthsci.utas.edu.au/hls/teaching/micro/mma.html Acid fast stain demonstrating chording Microscopy • Phase Contrast Microscopy – shift in light allows visualization of organism; can visualize viable organisms • Fluorescent Microscopy – certain dyes (fluorochromes) give off light when excited (fluorescence) – color of light depends on the dye and the filters used – Staining techniques • Fluorochroming: direct chemical interaction with organism – Acridine orange: stains nucleic acid; useful for cell-wall deficient organisms – Auramine-rhodamine: bind to mycolic acids in nearly all Mycobacteria – calcofluor white: binds to chitin in cell walls of fungi • Immunofluorescence: fluorochrome is bound to an antibody; can detect/identify specific organisms http://aeneary.myweb.uga.edu/lepto_files/image013.gif WBC nuclei Bacteria Staphylococci, acridine orange stain http://www.med.sc.edu:85/fox/strep-staph.htm Mycobacterium – auramine stain http://www.lung.ca/tb/abouttb/what/causes_tb.html Yeast—calcofluor white http://www.med.sc.edu:85/mycology/mycology-3.htm Mould—calcofluor white Influenza virus infected cells, fluorescent antibody stain Culture and isolation of bacteria • Principles of Cultivation – Nutritional requirements • General concepts – – • non-fastidious: simple requirements for growth fastidious: complex, unusual, or unique requirements for growth Phases of growth media – – solid agar; boil to dissolve, solidifies at 50ºC liquid, broth • Media classifications and functions – Enrichment • used to enhance growth of specific organisms – Supportive • support growth of most non-fastidious organisms – Selective • contains agents that inhibit the growth of all agents except that being sought (dyes, bile salts, alcohols, acids, antibiotics) – Differential • contains factor(s) that allow certain organisms to exhibit different metabolic characteristics • Types of artificial media – Brain-heart infusion • nutritionally rich supportive media used in broths, blood culture systems and susceptibility testing – Sheep blood agar • supportive media containing 5% sheep blood for visualization of hemolysis – Chocolate agar • same as sheep blood agar except blood has been “chocolatized” RBCs lysed by heating; releases X (hemin) and V (NAD) factors for Neisseria and Haemophilus – MacConkey agar • selective for Gram-negative rods (GNRs) because of crystal violet and bile salts; differential due to lactose, fermenters lower pH changing neutral red indicator pink/red • Types of artificial media – Hektoen enteric agar • – Columbia colistin-nalidixic acid (CNA) agar • – Columbia agar base, sheep blood, colistin and nalidixic acid; selective isolation of gram-positive cocci Thayer-Martin agar • • contains bile salts and dyes (bromothymol blue and acid fuchsin) to inhibit non-pathogenic GNRs; non pathogens ferment lactose changing BTB to orange; pathogens Salmonella and Shigella are clear; ferric ammonium citrate detects H2S production of Salmonella (black colonies) CAP with antibiotics (colistin inhibits gram neg, vancomycin inhibits gram pos, nystatin inhibits yeast); for N. gonorrhoeae and N. meningitidis; Martin-Lewis has similar function but different antibiotics Preparation of artificial media – Sterilization • autoclave: pressurized steam at 121ºC for 15-30 min. http://science.nhmccd.edu/biol/wellmeyer/media/media.htm Chocolate agar Uninoculated Haemophilus http://www.hardydiagnostics.com/catalog2/hugo/ChocolateAgar.htm MacConkey agar http://science.nhmccd.edu/biol/wellmeyer/media/media.htm Hektoen agar http://medic.med.uth.tmc.edu/path/hekto.htm • Environmental requirements – Oxygen and Carbon dioxide availability • • • • aerobic: room air facultative: aerobic or anaerobic microaerophilic: reduced oxygen tension anaerobic – • – strict or aerotolerant capnophilic: increased C02 (5-10%) Temperature • • • • 35-37ºC 30ºC cold 42ºC • Bacterial Cultivation – Isolation of bacteria from specimens • streaking for isolation • streaking for quantitation – Evaluation of colony morphologies • Type of media supporting growth • Relative quantities of each colony type • Colony characteristics – colony form: pinpoint, circular, filamentous, irregular – colony elevation: flat, raised, convex – colony margin: smooth, irregular • Gram stain and subcultures – sterile loop, isolated colonies Conventional methods for ID • Principles of Identification – ID using genotypic criteria – ID using phenotypic criteria • Microscopic morphology and staining characteristics • Colony morphology • Environmental requirements for growth • Resistance or susceptibility to antimicrobial agents – bacitracin, novobicin, vancomycin • Nutritional requirements and metabolic capabilities – Single enzyme tests • Catalase: H2O2 + catalase = O2 and H20; differentiates Staphylococcus v. Streptococcus, Listeria and corynebacteria v. other non spore forming gram-positive bacilli • Oxidase: detection of cytochrome oxidase that participates in nitrate metabolism; Pseudomonas, Aeromonas, Neisseria • Indole: tryptophanase degrades tryptophan into pyruvic acid, ammonia, and indole; indole is detected by aldehyde indicator; presumptive id for E. coli • Urease: hydrolyzes urea into ammonia, water and CO2; increase pH changes causes bright pink color of indicator • PYR: hydrolysis of PYR, indicator turns pink; Group A Strep and enterococci are + – Tests for presence of metabolic pathways • Oxidation and fermentation: oxidation of glucose requires oxygen, fermentation does not; pH decreases causing yellow color • Amino acid degredation: detection of amino acid decarboxylase enzymes O-F glucose media http://academic.mwsc.edu/jcbaker/bio390sec01/bio390_laboratory_study_images.htm • Principles of Phenotype-based ID schemes – Selection and inoculation of ID test battery • Type of bacteria to be identified • Clinical significance of isolate • Availability of reliable testing methods – Incubation for substrate utilization • Conventional ID • Rapid ID – Detection of metabolic activity • Colorimetry: pH change of indicators • Fluorescence: release of fluorophore from substrate or changes in fluorescence due to pH changes • Turbiditiy: growth or no-growth – Analysis of metabolic profiles • ID databases • Use of databases to ID unknowns – Confidence in ID API strips – bioMerieux • Commercial ID systems – Advantages and examples of commercial systems • • • • ARIS (Trek) MicroScan (Dade-Behring/Seimens) Phoenix (Becton-Dickinson) Vitek (bioMérieux) VITEK 2 bioMérieux Microscan Dade Behring Immunochemical methods for ID • Principles of immunochemical methods – Particle agglutination • Latex agglutination – Immunofluorescent assays • Direct immunofluorescence assay (DFA) • Indirect immunofluorescence assay (IFA) • Enzyme immunoassays – Solid-phase immunoassays • Membrane bound immunoassays • Immunochromatographic assays – Optical immunoassays Latex agglutination Lateral flow immunoassay Serologic methods for diagnosis • Features of the Immune Response – Characteristics of antibodies • Features of immune response useful in diagnostic testing – – – – Acute v. anamnestic response IgM v. IgG IgM can’t cross placenta immunocompetent v. immunocompromised • Interpretation of serologic tests – single v. paired sera; rare pathogen – 4-fold rise in titer v. qualitative testing – cross reactivity (herpes viruses, heterophile Abs, pregnancy) • Principles of Serologic Test Methods – Methods for antibody detection • Direct whole pathogen agglutination assays – pos patient sera causes organism to clump • Particle agglutination tests – latex beads or RBCs coated with Ag • Flocculation tests – RPR – precipitation of soluble Ag with Ab » charcoal particles coated with cardiolipin-lecithin binds reagin • ELISAs • IFAs – organism/antigen on slides; patient Ab detected with fluorescent secondary Ab • Western blots ELISA Western Blot