Chapter 3: DECALCIFICATION
advertisement

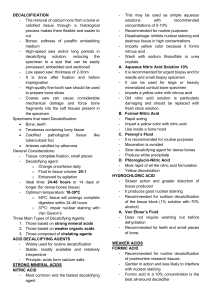
CHAPTER 3 DECALCIFICATION Learning Objectives: At the end of this chapter, students should know the decalcification of hard bony tissues. Specifically, to; 1. Define decalcification. 2. Discuss the importance of decalcification. 3. Determine and discuss the steps before decalcification. 4. Know the types of decalcification process. 5. Know the characteristics of an ideal decalcifying agent. 6. Discuss the application, advantages and disadvantages of each decalcifying process and the agents used; A. Mineral Acids B. Ion Exchange Resins C. Chelation D. Electrolytic 7. 8. Know the block surface decalcification. Know and discuss the decalcification end point determination methods. regie DECALCIFICATION • Decalcification is a process of complete removal of calcium salt from the tissues like bone and teeth and other calcified tissues (E.G. tuberculous lungs, arterioschlerotic vessels) after fixation. • Decalcification is done to assure that the specimen is soft enough to allow cutting with the microtome knife. • Unless the tissues is completely decalcified, sections will be torn and ragged and may damage the cutting edge of microtome knife,. regie 2 STEPS BEFORE DECALCIFICATION 1. Slice tissue samples at about 4-5 mm thick. Calcified tissue needs 2-3 hours only, for complete decalcification. Slice Tissue 2. Fixative of choice for bone or bone marrow is Zenker formal or Bouin's fluid. Unfixed tissue tends to be damaged 4 times greater during decalcification than a properly fixed tissue. Fix 3 DECALCIFICATION PROCESS TYPES 1. Dissolution of calcium by a diluted mineral ACID. 2. Removal of calcium by diluted mineral with ION EXCHANGE RESIN to keep the decalcifying fluid calcium free. 3. Using Chelating agents (EDTA) MINERAL ACID ION EXCHANGE RESIN DECAL CIFICA TION CHELATING AGENT ELECTRICAL CURRENT 4. Electrolytic removal of calcium ions from tissue by use of ELECTRIC CURRENT. regie 4 GOOD DECALCIFYING AGENT CRITERIA 1. Completely removal of calcium. 2. Absence of damage to tissue cells. 3. Subsequent staining not altered. 4. Shorter time. regie 5 MINERAL ACIDS MINERAL ACIDS: A. STRONG ACID (Nitric Acid , Hydrochloric Acid) B. WEAK ACID (Formic Acid, Acetic Acid, Picric Acid) Nitric Hydro chloric CALCIUM Formic dissolution Picric Acetic • NITRIC ACID: Very rapid, but if used for longer than 24-48 hours cause deterioration of stainability specially of the nucleus. Choice for temporal bones. Example: 1. PERENYI’S FLUID (nitric acid, absolute alcohol, chromic acid) Slow for decalcifying hard bone but excellent fluid for small deposits of calcium eg. calcified arteries, coin lesions and calcified glands. 2. Formalin Nitric acid Nitric acid causes serious deterioration of nuclear stainability which partially inhibited by formaldehyde. MINERAL ACIDS • HYDROCHLORIC ACID: Slower than nitric acid but still rapid. Fairly good nuclear staining. • FORMIC ACID: Extensively used as acid decalcifier. Nuclear staining in better, but requires neutralization and thorough washing prior to dehydration. Example: 1. Gooding and Stelwart's fluid. (Formic acid, Formalin) 2. Evans Krajian fluid (Trisodium citrate, formic acid). At pH 2-3. 3. Formic Acid Sodium Citrate - Gives better staining result than nitric acid method, since its less harsh on the cellular properties. Therefore even with over exposure of tissue, it causes little loss of staining qualities. 7 SURFACE DECALCIFICATION The surface of the block to be decalcified is trimmed with scalpel. The block is then placed in acid solution at 1% hydrochloric acid face downwards. 8 ION EXCHANGE RESINS • ION EXCHANGE RESINS are used to remove calcium ion FROM FLUID. • The resins is an ammoniated salt of sulfonated resin along with various concentrations of formic acid are used. • After use, the resin may be regenerated by with dilute N/10 HCL followed by distilled water. • ADVANTAGES: 1. faster decalcification 2. tissue preservation 3. cellular details better preserved 9 CHELATING AGENTS CHELATING AGENTS are organic compounds which binds certain metals. Ethylene-diamene-tetraacetic acid, disodium salt called VERSENATE has the power of capturing calcium. This is a slow process but has little or no effect on other tissue elements. Some enzymes are still active after EDTA decalcification. 10 ELECTROLYTIC AGENT • Electrolytic method the electrolyte APPARATUS attracts calcium ions to a negative electrode with added decalcifying solution (HCL, Formic acid, Distilled water). FOLLOW-UP STEPS: 1. Neutralization: tissues are de-acidified or neutralized by treatment with alkali (lithium or sodium sulphate). 2. Washing: removes acid or alkali which would otherwise interfere with staining. regie 11 DECALCIFICATION END POINT DETERMINATION METHODS 1. FLEXIBILITY Bending, needling or by use of scalpel if it bends easily that means decalcification is complete. This is unreliable, and may cause damage and distortion. 2. X-RAY Best method but very costly. Tissue fixed in mercuric chloride containing fixatives cannot be tested as they will be radio opaque. 3. CHEMICAL It is done to detect calcium FROM the decalcifying fluid. If calcium is tested negative, decalcification in considered complete. regie 12