Non-Protein Nitrogen(NPN) Compounds
advertisement
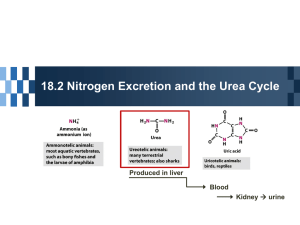
UG3, Semester 5 Clinical Biochemistry Lecture 3 Non-Protein Nitrogen(NPN) Compounds Non-protein Nitrogen Compounds • The determination of nonprotein nitrogenous substances in the blood has traditionally been used to monitor renal function. • Nitrogen containing compounds that are not proteins or polypeptides • Useful clinical information is obtained from individual components of NPN fraction Clinically Significant NPN • The NPN fraction comprises about 15 compounds • Majority of these compounds arise from catabolism of proteins and nucleic acids Urea Nitrogen (Blood) BUN • Highest concentration of NPN in blood • Major excretory product of protein metabolism • These processes release nitrogen, which is converted to ammonia • Synthesized in the liver from CO2 and Ammonia that arises from deamination of amino acids Urea Nitrogen (Blood) BUN • Assays for urea were based on measurement of nitrogen, the term blood urea nitrogen (BUN) has been used to refer to urea determination. • Excreted by the kidneys – 40% reabsorbed • <10% of the total are excreted through the gastrointestinal tract and skin. • Concentration is determined by: – Renal function – Dietary intake – Protein catabolism rate Clinical Application • Measurement of urea is used to: – evaluate renal function, – to assess hydration status, – to determine nitrogen balance, – to aid in the diagnosis of renal disease, – and to verify adequacy of dialysis. Disease Correlations • Azotemia: elevated conc. of urea in blood • Very high plasma urea concentration accompanied by renal failure is called uremia, or the uremic syndrome • Causes of urea plasma elevations are: – Prerenal – Renal – and postrenal Pre-Renal Azotemia • Reduced renal blood flow Less blood is delivered to the kidney less urea filtered – Anything that produces a decrease in functional blood volume, include: • • • • Congestive heart failure, shock, hemorrhage, dehydration • High protein diet or increased catabolism (Fever, major illness, stress) Renal Azotemia • Decreased renal function causes increased blood urea due to poor excretion – Acute & Chronic renal failure – Glomerular nephritis – Tubular necrosis – & other Intrinsic renal disease Post-Renal Azotemia • Obstruction of urine flow –Renal calculi • Tumors of bladder or prostate • Severe infections Decreased Urea Nitrogen • • • • Low protein dietary intake Liver disease (lack of synthesis) Severe vomiting and/or diarrhea (loss) Increase protein synthesis Analytical methods • Assays for urea were based on measuring the amount of nitrogen in the sample (BUN) • Current analytic methods have retained this custom and urea often is reported in terms of nitrogen concentration rather than urea concentration (urea nitrogen). • Urea nitrogen concentration can be converted to urea concentration by multiplying by 2.14 Analytical methods • Urease → hydrolysis of urea to ammonium ion , then detect ammonium ion (NH4+) • Enzymatic – The most common method couples the urease reaction with glutamate dehydrogenase Analytical methods Indicator dye NH4+ + pH indicator → color change Conductimetric ◦ Conversion of unionized urea to NH4+ and CO32- results in increased conductivity Reference range of Urea N: Serum or plasma: 6-20 mg/dl 24 hours Urine: 12-20 g/day