Cell injury and cell responses
advertisement

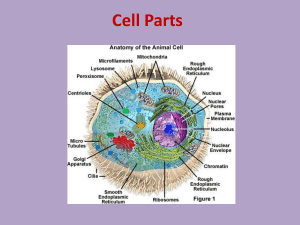
Dr. Temur Ahsan Khan Cells and tissues undergo a number of responses according to intensity and duration of pathological conditions and injuries 1. Cellular adaptations-----hypertrophy, atrophy, hyperplasia, metaplasia etc 2. Regressive changes (degeneration)---swelling (hydropic degeneration) and steatosis (fatty Change) 3. Cell death (necrosis) and apoptosis (programmed cell death) 1. 2. 3. 4. Coagulative Liquefactive or lytic Caseous Fat necrosis 1. 2. 3. Same as general causes of disease. A very common cause of cell injury is hypoxia and anoxia (ischemia) Combination of hypoxia /anoxia are: Anoxic anoxia---inadequate oxygen in the presence of circulation for example in anaemia, pneumonia, liver necrosis, congestion etc. Ischemic anoxia---due to decrease or stoppage of arterial blood flow as in embolism, thrombism and infarction. Cytoxic anoxia---there is interference with O2 utilization as seen in cyanide poisoning. Sensitivity to anoxia varies in different tissues, for example following loss of blood supply neurons die within 3-5 minutes, myocardium, hepatocytes and several epithelial cells between 30 minutes to two hours and fibroblasts, epidermis and skeletal muscles survive for several hours. 1. 2. 3. 4. Plasma membranes---cause leakage Mitochondria---depletion of ATP Synthesis of proteins in rough endoplasmic reticulum is stopped. Preservation of integrity of genetic apparatus is compromised. ATP depletion (a) All energy requiring functions stop, H2O, Na+ and Ca2+ go inside the cell and K+ comes out. (b) Energy is derived through anaerobic glycolysis which causes accumulation of lactic acid and lowering of pH. 1. 2.Generation of oxygen derived free radicals Supereoxide anion, hydroxyl radical, hydrogen peroxide, nitric oxide, carbon tetrachloride. Volatile and tissue destructive. Important mechanism in radiation injury, killing of bacteria by leucocytes etc. Generated during metabolism of oxygen and mitochondrial electron transport. Free radicals oxidize proteins, membranes, genetic material and unsaturated fatty acidsperoxidation of fat—autocatalysis Antioxidants– superoxide dismutase, hydrogen peroxide, catalase, glutathione peroxidase, selenium and vitamin E Oxidative stress: imbalance between free radical generation and their removal / inactivation. 3. Loss of calcium homeostasis: accumulation of calcium in cytosol has the following serious consequences and eventually causes cell death: (a) uncoupling of gap junctions, isolation and dissociation of injured cells (b) depolymerization of cytoskeleton i.e. micrifilaments and microtubules. Cytoskeleton disappears from the periphery of the cell. The cell cannot perform its function of movement, phagocytosis and secretion and it looses shape (become rounded) (c) activation of endogenous phospholipases which cause breakdown of cell membranes. 4. defects in membrane permeability Caused directly by bacterial toxins, viral proteins, complement components and cytoxic lymphocytes etc. Caused indirectly by loss of ATP and enzymes activated by Ca2+ like phospholipases 5. mitochondrial damage Several mechanisms Increased cytosolic Ca2+ and oxidative stress Formation of high conductance channels As the injured cell die, proteins and other large molecules present in the cell escape into the interstitium and then into the blood circulation. Necrosis in the following tissues releases specific enzymes into the blood and these can be assayed to determine the extent of damage: Heart---creatine kinase (CK) Skeletal muscle---asparatate aminotransferase (AST) and CK isoform Liver ---alanine aminotransferase (ALT) and AST Pancreas---pancreatic specific lipase. General Pathology (PATH 303) Lecture # 4 Common Biochemical Mechanisms of Cell Injury (Contd.) 1. Mechanisms of injury caused by free radicals: Lipid peroxidation of plasma and cell membranes Attack double bond in unsaturated fatty acids Autocatalytic chain reaction Cross-linking of proteins Inactivate sulphydryl enzymes Form disulphide bonds DNA fragmentation React on thymine in DNA Cause mutation and fragmentation 2. Loss of calcium homeostasis Increase in cytosolic Ca o o Influx from outside Release from mitochondria Activates phospholipase, protease, ATPase, endonuclease Depolymerization of cytoskeleton Inhibits cell movement Inhibits phagocytosis Inhibits secretion 3. Defects in membrane permeability Directly damaged by: o Bacterial toxins Viral proteins Complement component Cytotoxic lymphocytes etc. Indirectly damaged by: o o o Loss of ATP synthesis Activation of phospholipase by Ca 4. Mitochondrial damage Irreparable damage to mitochondria causes cell death. By increased cytosolic Ca, oxidative stress, breakdown of phospholipids. Formation of high conductive channels Leakage of proteins and cytochrome C 5. Lysosomes, heterophagy and autophagy Primary lysosomes contain hydrolytic enzymes Fuse with phagosomes to produce phagolysosomes and cause break down of ingested material Heterophagy --- endocytosis of particulate matter from outside e.g. bacteria; --- pinocytosis – uptake of soluble macromolecules. Autophagy: Removal of damaged or senescent organelles by autophagic vacuoles formed from RER. Fuse to form autophagolysosomes. 6. Cellular swelling Disturbance of cellular metabolism leads to cellular swelling. Causes: Toxins, temperature, metabolic diseases, poisons, hypoxia Gross appearance: Organ enlarged, increased weight, edges become rounded, cut surface bulges, capsule retracts. Microscopic appearance: Seen in cells of liver, kidney, cardiac and skeletal muscles. Cells are larger in size. Cytoplasm stains darker and appears granular. Significance: Reversible caused by mild injury--disappears when the cause is removed. 7. Hydropic degeneration Similar to but more severe than acute cellular swelling. Water enters the cells and dilutes cytoplasm. Protease clears the cytoplasm. Causes: Mechanical (rubbing) injuries, thermal injuries, chemical agents; infectious agents - some neoplasm. Grossly: Blisters are circumscribed, raised area, fluctuating, filled with fluid Microscopic: Water accumulates in endoplasmic reticulum forming clear vacuoles, ballooning degeneration - Fuse and rupture to form bullae and vesicles. Significance: If uncomplicated, it heals quickly without scar formation. Secondary infections cause abscessation.