Power Point CH 21
advertisement

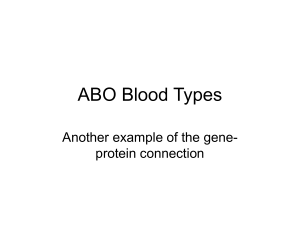
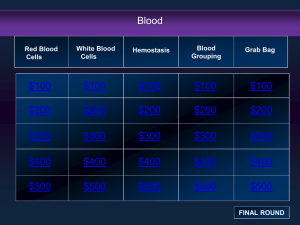
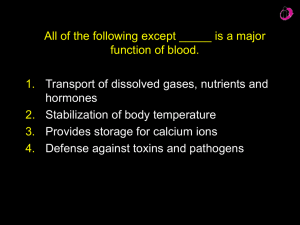
Chapter 21 *Lecture Outline *See separate FlexArt PowerPoint slides for all figures and tables pre-inserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Chapter 21 Outline • General Composition and Functions of Blood • Blood Plasma • Formed Elements in the Blood • Hemopoiesis: Production of Formed Elements Introduction Blood serves many functions. Some examples are: • Transportation of oxygen and carbon dioxide as well as nutrients and waste products • Regulation of body temperature, pH, and fluid volume • Protection by mounting an immune response and the production of antibodies Composition of Blood Figure 21.1 Composition of Blood Upon separation by centrifugation, blood has three factions: 1. Erythrocytes—represent ~ 44% of total blood volume 2. Buffy coat—represents about 1% of total blood volume 3. Plasma—represents ~ 55% of total blood volume Composition of Blood Figure 21.2 Blood Smear Figure 21.3 Blood Plasma Formed Elements • The hematocrit is the % of the volume of all formed elements in one’s blood • It varies in females from 38%–46% and between 42%–56% in males Erythrocytes • Also referred to as red blood cells or RBCs, but this is a misnomer as mature RBCs lack nuclei and other organelles Figure 21.4 Erythrocytes • Relatively small (7.5 μm in diameter) • Unique biconcave shape • As they pass through small blood vessels, they line up in single file termed a rouleau Hemoglobin in Erythrocytes • • • Every erythrocyte contains 280 million molecules of a red-pigmented protein called hemoglobin Hemoglobin is capable of reversibly transporting oxygen and carbon dioxide in the blood Hemoglobin consists of four globin protein molecules: 1. 2. Two alpha (α) chains Two beta (ß) chains Molecular Structure of Hemoglobin Figure 21.5 Hemoglobin • Each of the four globins possesses a nonprotein heme group containing an iron (Fe2+) molecule. • Each hemoglobin molecule can bind a combination of four oxygen/carbon dioxide molecules. Recycling the Components of Aged or Damaged Erythrocytes Figure 21.6 Blood Type Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. ABO Blood Types Antigen A Antigen B Antigens A and B Neither antigen A nor B Erythrocytes Anti-B antibodies Anti-A antibodies Neither anti-A nor anti-B antibodies Both anti-A and anti-B antibodies Plasma Blood type Type A Erythrocytes with type A surface antigens and plasma with anti-B antibodies Type B Erythrocytes with type B surface antigens and plasma with anti-A antibodies (a) Rh Blood Types Antigen D No antigen D Erythrocytes No anti-D antibodies Anti-D antibodies (after prior exposure) Rh positive Erythrocytes with type D surface antigens and plasma with no anti-D antibodies Rh negative Erythrocytes with no type D surface antigens and plasma with anti-D antibodies, only if there has been prior exposure to Rh positive blood Plasma Blood type Figure 21.7 (b) Type AB Erythrocytes with both type A and type B surface antigens, and plasma with neither anti-A nor anti-B antibodies Type O Erythrocytes with neither type A nor type B surface antigens, but plasma with both anti-A and anti-B antibodies Agglutination Reaction Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. + Donor blood type = Recipient blood type Agglutination reaction Antigen A + Type A blood of donor (has surface antigenA) = Type A blood of recipient (contains anti-B antibodies) Antigen and antibody do not match No clumping seen. Successful blood type match. No agglutination Antigen A + Type A blood of donor (has surface antigenA) = Type B blood of recipient (contains anti-A antibodies) Antigen and antibody match and connect Agglutination Clumping seen. Hemolysis occurs. Unsuccessful blood type match. (a) Agglutination test Type B recipient erythrocyte Blood from type A donor Anti-A antibody in recipient plasma Type A donor erythrocyte Agglutinated erythrocytes from type A donor block small vessels Figure 21.8 (b) Erythrocyte agglutination a: © Jean Claude Revy-ISM/Phototake Leukocytes • Unlike erythrocytes, leukocytes possess a nucleus and organelles. • They help initiate an immune response and defend the body against pathogens. • They are 1.5 to 3 times larger than erythrocytes. • They are capable of leaving the blood vessels, diapedesis, and entering a tissue. • Leukocytes are attracted to a site of infection by molecules from damaged cells or invading pathogens. This attraction is called chemotaxis. Classification of Leukocytes • The five types of leukocytes are divided into two classes (granulocytes and agranulocytes) based on the presence or absence of visible organelles termed granules. Leukocytes Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Table 21.3 Leukocytes LM 1600x Eosinophil LM 1600x LM 1600x Neutrophil Basophil Granulocytes Agranulocytes LM 1600x LM 1600x Lymphocyte Type GRANULOCYTES Monocyte Characteristics Functions Approximate % Neutrophils Nucleus is multilobed (as many as five lobes) Cytoplasm contains neutral or pale, distinct granules (when stained) Phagocytize pathogens, especially bacteria Release enzymes that target pathogens 50–70% of total leukocytes Eosinophils Nucleus is bilobed Phagocytize antigen-antibody complexes and allergens 1–4% of total leukocytes Cytoplasm contains reddish or pink-orange granules (when stained) Basophils Nucleus is bilobed Cytoplasm contains deep blue-violet granules (when stained) Release chemical mediators to destroy parasitic worms Release histamine (vasodilator) and heparin (anticoagulant) during inflammatory or allergic reactions 0.5–1% of total leukocytes AGRANULOCYTES Lymphocytes Round or slightly indented nucleus (fills the cell in smaller lymphocytes) Nucleus is usually darkly stained Thin rim of cytoplasm surrounds nucleus Attack pathogens and abnormal/infected cells Coordinate immune cell activity Produce antibodies 20–40% of total leukocytes Monocytes Kidney-shaped or C-shaped nucleus Nucleus is generally pale staining Abundant cytoplasm around nucleus Can exit blood vessels and become macrophages Phagocytize pathogens, cellular debris, dead cells 2–8% of total leukocytes Platelets • Irregular membrane-enclosed cellular fragments that represent shed cytoplasm from cells in the red bone marrow called megakaryocytes • Megakaryocytes are about 15× larger than erythrocytes • Platelets are about ¼ the size of erythrocytes • Platelets are involved in the clotting of blood Platelets and Megakaryocytes Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Red bone marrow Megakaryocyte Megakaryocytes LM 1600x Endothelial cells (a) (b) a: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Figure 21.9 Proplatelets Platelets Blood Clot Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Fibrin Platelets Erythrocytes SEM 4100x Reprinted by permission from Macmillan Publishers Ltd: Nature, Dr. John W. Weisel and Yuri Veklich. Vol. 413, Issue 4, Cover Image, October 2001. © 2001 Nature Publishing Group Figure 21.10 Hemopoiesis Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Hemocytoblast (blood stem cell) Lymphoid line Myeloid line Myeloid stem cell Multi-CSF Lymphoid stem cell Multi-CSF Multi-CSF Erythropoiesis Progenitor cell Thrombopoiesis Leukopoiesis Progenitor cell B-lymphoblast GM-CSF T-lymphoblast Progenitor cell Proerythroblast Megakaryoblast Myeloblast M-CSF Monoblast EPO Early erythroblast Thrombopoietin G-CSF Promegakaryocyte Promyelocytes Late erythroblast M-CSF Promonocyte Thrombopoietin Normoblast Megakaryocyte Eosinophilic myelocyte Basophilic myelocyte Neutrophilic myelocyte Eosinophil Basophil Neutrophil Nucleus ejected Reticulocyte Erythrocyte Thrombopoietin Platelets Figure 21.11 Monocyte B-lymphocyte T-lymphocyte Erythropoiesis • Erythropoiesis is the process of erythrocyte production. • About 3 million erythrocytes are produced per second. • During maturation all organelles within the erythrocyte, including the nucleus, degenerate leaving the erythrocyte with nothing more than a “bag of hemoglobin.”