CHEMOPREVENTION
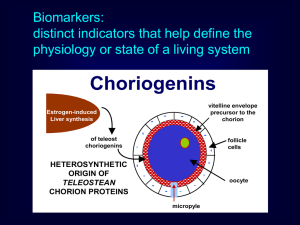
advertisement

CHEMOPREVENTION: PRINCIPLES AND PROSPECTS Gary D. Stoner, Ph.D. Department of Internal Medicine College of Medicine and Public Health The Ohio State University Strategies for Cancer Prevention • Reduce Exposure to Environmental • Carcinogens Identify Individuals at High Risk • Genetic factors • Biochemical factors • Chemoprevention • Dietary factors • Synthetic agents Chemoprevention The prevention of cancer development by dietary or synthetic chemicals Chemoprevention Drug Development Preclinical: Natural Products Synthetic Agents In vitro Assays Antimutagenic Cell Transformation etc. In vivo assays Clinical: Phase I Phase II Phase III Tumors Toxicity Efficacy Efficacy Biomarkers Metabolism Biomarkers Cancer Toxicology Endpoint Qualities of an Ideal Chemopreventive Agent Chemopreventive Agents • • • • • • • Allyl sulfides Calcium Coumarins Dithiolethiones Indoles Isoflavones Isothiocyanates • • • • • • • Monoterpenes NSAIDs Polyphenols Protease inhibitors Retinoids Selenium Vitamins (A, C, D3,E) Classes of Chemopreventive Agents “Blocking” agents • Inhibitors of tumor initiation “Suppressing” agents • Inhibitors of tumor promotion/ progression Blocking (Anti-Initiating) Agents • Influence metabolic activation of carcinogens • Deactivate/detoxify carcinogens • Scavenge electrophiles and oxygen radicals • Increase level of fidelity of DNA repair Carcinogen Metabolism Carcinogen Activation Genetic (DNA) Damage Detoxification Conjugates Excreted Cancer Agents That Influence Carcinogen Activation Mechanism Examples Inhibition of cytochrome dithiocarbamates P450 ellagic acid diallyl sulfide isothiocyanates Induction of cytochrome P450 M.A. Morse and G.D. Stoner, 1993 indole-3-carbinol -naphthoflavone Isothiocyanates N N CH3 N=C=S O N-Nitrosomethylbenzylamine (NMBA) 3-Phenylpropyl isothiocyanate (PPITC) N=C=S N=C=S Benzyl isothiocyanate (BITC) N=C=S Phenethyl isothiocyanate (PEITC) 4-Phenylbutyl isothiocyanate (PBITC) N=C=S 6-Phenylhexyl isothiocyanate (PHITC) NMBA Metabolism O (NMBA) H3C N CH2 cytochrome p450 O N OH -hydroxynitrosamine H3C N CH H C O methyldiazohydroxide [ CH3N = NOH ] benzaldehyde methyldiazonium ion [ CH3+N N ] carbonium ion [ CH3+] O NH H2N N OCH3 CH3 N N R N7-Methylguanine N N H2N N N R O6-Methylguanine Protocol For Identification of Blocking Agents in Rat Esophagus NMBA (1x/wk/15 wks) 0 2 4 19 Inhibitor 25 Effect of Isothiocyanates on DNA Methylation and Tumorigenesis in Rat Esophagus O6-Methylguanine Treatment (mol/mol guanine) Tumors / Rat NMBA 19.6 0.6 7.2 0.7 NMBA + BITC 16.0 0.4 6.5 0.6 NMBA + PEITC 2.1 0.2a 0.1 0.1a NMBA + PPITC 3.0 0.3a 0.0 0.0a NMBA + PBITC 7.0 0.6a 4.0 0.4 NMBA + PHITC 20.7 1.0 11.9 0.7a ap < 0.05 Agents That Deactivate/Detoxify Carcinogens Mechanism Introduction of phase II enzymes • glutathione-Stransferases • UDP-glucuronyltransferases • glutathione peroxidase Examples • allyl sulfides, dithioethiones, isothiocyanates • polyphenols • selenium O S H3C N C S Sulforaphane Y. Zhang, P. Talalay, C.G. Cho, and G.H. Posner, A major inducer of anticarcinogenic protective enzymes from broccoli: isolation and elucidation of structure. Proc Natl Acad Sci USA 89 2399 (1992) Induction of QR and GST in Mouse Tissues by Sulforaphane* (15 mol / mouse / day) Liver Forestomach Small Intestine Lung QR 2.45 0.07 1.70 0.18 2.34 0.19 1.37 0.14 GST 1.86 0.08 1.98 0.08 2.13 0.20 1.17 0.09 Enzyme QR = Quinone reductase GST = Glutathione-S-transferase Protective Effects of Sulforaphane on DMBA-Induced Mammary Tumors in Rats* Treatment Control Tumor Incidence (% of control) Tumor Muliplicity Tumor Weight (% of control) (gm) (% of control) 65.2 (100) 1.43 (100) 2.79 (100) 75 mol 35.0 (53.8) 0.45 (31.4) 1.24 (44.4) 150 mol 26.3 (40.3) 0.26 (18.2) 0.68 (24.4) Sulforaphane *Y.Zhang, PNAS 91: 3147, 1994 Suppressing Agents • Inhibit cell growth • Stimulate cell function • Stimulate apoptosis • Inhibit blood vessel formation (angiogenesis) POLYAMINE SYNTHESIS Ornithine ODC Putrescine Spermidine Carbon dioxide Chemopreventive Agents: a. difluromethylornithine (DFMO) b. curcumin Spermine DFMO as an Anti-Tumor Agent Azoxymethane-induced rat colon tumor model • • • inhibits tumor incidence and multiplicity decreases cell proliferation decreases activated ras expression NMBA-induced rat esophagus model • inhibits tumorigenesis when given before, during and after NMBA • decreases cell proliferation and increases apoptosis Human Neoplasias • Barrett’s esophagus; colonic polyps; oral leukoplakia; uterine cervix (CIN 3) Action of COX Enzymes COOH Arachidonic Acid Cyclooxygenase Activity COX-1 COX-2 PGG2 Peroxidase Activity PGH2 Prostacyclin PCI2 Prostaglandins PGE2, PGF2, PGD2 Thromboxane TxA2 Inhibitors of COX Activity NSAIDs • Aspirin, Indomethacin, Ibuprofen, Naproxen • Effective chemoprevention agents in rodent skin, breast and colon tumor models • Aspirin may be effective as a prevention agent in human esophageal cancer Selective COX-2 inhibitors • Celecoxib, Rofecoxib and others • Animal studies indicate that these agents are as effective and better tolerated than NSAIDs COX Activity and Human Cancers Human Breast • Elevated COX-2 activity is seen in tumors • NSAID use is associated with reduction in susceptibility to breast cancer (Robertson, Harris) Human Colon • Colon polyps have elevated COX-2 activity • Treatment of FAP patients with Celecoxib leads to polyp regression Transcription factors Growth factor receptor Other stimuli Elevated ROS levels ras ceramide Elevated NFkB activity raf MEK-1 Erks Elevated AP-1 activity Altered gene expression Increased cell proliferation, resistance to apoptosis Transcription Factors and Tumorigenicity AP-1 • Regulates transcription of genes involved • • • in cell proliferation, differentiation and modulation of extracellular matrix Elevated AP-1 activity is causally related to tumor promotion and progression in the mouse skin model Agents that inhibit AP-1 activity, such as retinoids, are effective chemoprevention agents in this model The role of altered AP-1 activity in other epithelial tumors is unknown at present Transcription Factors and Tumorigenicity NFkB • Elevated activity seen in mouse skin • • • model Elevated in human Barrett’s esophagus and esophageal cancers In cell culture models, elevated NFkB activity correlates with increased resistance to apoptosis Selective inhibitors of NFkB activity are unavailable at present Tumor Angiogenesis • Neovascularization is essential for sustained tumor growth as well as establishment of metastases. • Anti-angiogenesis factors include endostatin, a product of plasminogen, that inhibits new vessel growth in tumor xenografts in mice. Endostatin is presently being evaluated in human clinical trials for its efficacy against metastatic disease. Human Clinical Trials Phase I • Toxicity, metabolism Phase II • Biomarkers Phase III • Long term prospective studies Target Populations for Chemoprevention High Risk Individuals • Hereditary predisposition • High exposure to carcinogens • precancerous lesions • previous treatment for cancer General Population ? Chemoprevention Trials Evaluation • Modulation of Intermediate Endpoints (Biomarkers) • Prevention and/or Reversal of Precancerous Lesions • Extension of Latency Period for Cancer Development • Reduction of Cancer Incidence and Mortality Phase I Trials Population • Usually high risk • 18-24 subjects Escalating Dose Objectives • Determine pharmacokinetic parameters • Minimum and maximum tolerated dose • Time course of the reversibility of side effects • Dose selection for Phase II trials Phase I Clinical Trial of Freeze-Dried Black Raspberries • 10 normal volunteers, > 18 years of age • “Phenol-free” diet • 90 g BRB / day, 14 days • Blood and urine • Clinical signs of toxicity Results of Phase I Clinical Trial of Freeze-Dried Black Raspberries • Well tolerated • blood levels of ellagic acid and several anthocyanins • Reduced levels of 8-OH-dG in urine Phase II Trials Randomized placebo controlled Population • High risk • 100-200 subjects Objectives • Further evaluation of toxicity • Dose response vs. biomarker modulation • Dose selection for Phase III trials BIOMARKERS Anti-Initiation 1. Phase I enzyme activities 2. Phase II enzyme activities 3. DNA repair enzyme activities 4. DNA adducts (carcinogen and free radicals) 5. Hemoglobin adducts 6. Urinary metabolites • • Detoxification products Mutagenicity assays 7. Micronuclei, binucleated cells 8. Chromosome damage (FISH) BIOMARKERS Anti-Promotion/Progression 1. Proliferation Index: PCNA, Ki67, BrdU, 3H-thymidine 2. ODC activity; polyamine levels 3. Growth factor and receptor expression 4. Prostaglandin levels 5. Cell differentiation • Blood group antigens • Keratins • Retinoid receptors • Squamous metaplasia mucociliary differentiation 6. Apoptosis 7. Morphometric 1. DNA ploidy 2. Nuclear/nucleolar-morphology Barrett’s Esophagus Normal Barrett’s Esophagus Esophageal Cancer Multi-Center Clinical Trial Study Schema Barrett’s Esophagus Intestinal Type Metaplasia Low Grade Dysplasia Biopsies for Surrogate Endpoint for Biomarkers Randomize DFMO 900mg, Once Daily x 26 Weeks Placebo, Once Daily x 26 Weeks Endscopy with Biopsies for Endpoint Biomarkers Endoscopy with Biopsies for Endpoint Biomarkers 26 Weeks, No Treatment Endoscopy with Biopsies for Endpoint Biomarkers 26 Weeks, No Treatment Endoscopy with Biopsies for Endpoint Biomarkers Overall Study Objectives Determine if oral DFMO given in a randomized, placebo-controlled, double-blinded study will significantly alter: Primary Endpoint: Ki-67 labeling index Secondary Endpoints: p53 protein accumulation Levels of Cyclin D1, EGFR, or TGF-alpha DNA ploidy, nuclear and nucleolar morphometry Cellular apoptosis Pathology & morphology of Barrett’s Phase III Strategies • Target Populations • Length of Study • Conclusiveness of Study • Statistical Methods Combination Strategies • Synergistic Activity • Lower Doses of Each Lower Toxicity + Fewer Adverse Effects • Mechanistic Combination Strategy (Anti- Initiator/ Anti-Proliferator) Collaborators OSU OSU - Former Students Robeena Aziz Rajaram Gopalakrishnan Peter Carlton Leena Khare Tong Chen Laura Kresty Ashok Gupta Dian Wang Keith Harris Qian-Shu Wang Tamaro Hudson American Health Foundation Beth Liston Fung-Lung Chung Mark Morse Univ. of Minnesota Ron Nines Stephen Hecht Haiyan Qin Sharon Murphy