2011 RSV - Emory University Department of Pediatrics
advertisement

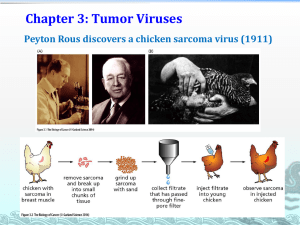
LOWER AIRWAY DISEASES Pediatric Critical Care Medicine Emory University Children’s Healthcare of Atlanta Objectives • Categories: – Bronchiolitis – Asthma • • • • • Epidemiology Etiology Pathophysiology Clinical manifestations Treatment Bronchiolitis: Etiology • Population <2yr: 1-3.5% admissions; 1-2% ER visits • Risk factors: prematurity, CLD or BPD, CHD, age 3-6 mos at the onset of the epidemic • Other risk factors: older sibs, day care, male, exposure to smoke & breast feeding < 2 months (lower socioeconomic pop) • RSV constituted ~ ½ of the cases; 20-25%- others; 9-27% coviral infections • Other viruses: rhinovirus, adenovirus, metapneumovirus, influenza, parainfluenza, enterovirus and bocavirus • RSV causes more symptoms with wheezing and retractions, longer duration of respiratory symptoms and oxygen therapy associated with lower use of antibiotics » Concensus conference on acute bronchiolitis; An Pediatri, 2010 Bronchiolitis • Bronchiolitis: a specific clinical symptom complex – <12 months old – Brief prodrome of URI followed by wheezing, dyspnea, respiratory distress, tachypnea, hyperinflation on CXR • Premature – Apneic spells, atelectasis/infiltrates and hyperinflation – May require oxygen supplementation and mechanical ventilation Respiratory Syncytial Virus (RSV) • First identified >50 yrs ago • 2 epidemics in the 1930s &1940s: describing the seasonal variability and physical and pathological manifestations of the disease without identified organisms • 1955: Walter Reed researchers isolated a virus from the nasal secretions of young chimpanzees named chimpanzee coryza agent (CCA) • 1956 Robert Chanock isolated CCA from 2 infants with characteristic mutinucleated giant cells within a large syncytium renamed “respiratory syncytial virus” RSV: Microbiology • Single strand RNA virus: Paramyxoviridae family, 10 genes encoding 11 proteins • 2 surface glycoproteins – Surface glycoprotein (G): mediates attachment to the host cells – Fusion protein (F): promotes aggregation of mutinucleated cells through fusion of their plasma membranes • Two distinct antigenic subgroups: A&B – G protein is responsible with 53% homology – Controversy over which subgroup caused more severe symptoms RSV: Epidemiology • #1 cause of pediatric bronchiolitis & asthma: 60% of all and 80% of <1yr old with acute LRTI; 10x mortality rate compared to influenza • Seasonal outbreak: in winter months, endemic in sub-tropic regions • All children have been infected by 2 yrs of age with 50% of >2 infections; infection doesn’t provide long term immunity • 40% infected develop LRTI; 2-5% required mechanical ventilation • Health burden world wide with mortality of 5% • Significant morbidity in premies (<35 week EGA, lacking placental IgG transfer), CLD and CHD • Peak incidence of severe illness is between 2-3 months of age • Also affect immunocompromized adults and the elderly RSV: Epidemiology • Mortality 0.005-0.02% in healthy children; 1-3% in hospitalized patients • Increase correlation with SIDS (25% of post mortem) probably related to prolonged apnea • Chronic sequelae: early life RSV infection is an independent risk factor for recurrent wheeze and asthma: 30-40% of likelihood of recurrent asthma-like episodes – Stein et al.: tapered off after 6 yrs and became insignificant after 13 yrs – Sigurs et al.: showed increased risk beyond 13 yrs RSV: Pathophysiology • Transmission – Direct contact of respiratory secretions to nasopharyngeal or conjunctival mucous membrane – Viable on hard surface (6 hrs); rubber gloves (90 min); skin (20 min) – Incubation: 2-8 days – Shedding • 3 weeks in immunocompetent • Several months in immunocompromised • Replication: in nasopharyngeal but most efficient in the bronchiolar epithelium – Direct spread – Hematogenously via monocytes – Causes: necrosis of the bronchiolar epithelium lymphocytic peribronchiolar infiltration & subsequent submucosal edema; mucus secretions increase in both quantity and viscosity RSV: Immune Response • “Master switch” of genetic control • RSV induce specific cell-mediated immune response: lymphocyte transformation, cytotoxic T-cell responses, & antibody-dependent cellular cytotoxicity responses RSV: Immune response Anatomy: direct tissue damage to the mucosa sloughing of the epithelium activate of irritant receptors neurogenic stimulation of bronchial smooth ms & development of spasm Up regulate substance P (neuropeptides) & density of its receptors (NK1) significant bronchoconstriction Nerve growth factor (NGF) regulate the development of peripheral afferent and efferent neurons change in the distribution and reactivity of sensory & motor nerves non specific airway hyper-reactivity Early respiratory infections may contribute to early systemic sensitization to other antigens & allergens Neuro-immune interaction via neurotrophic pathway resistant to corticosteroids RSV: Immune Response Infection produce both serum and mucosal IgM, IgA, IgG: act in protective role ◦ IgM: 5-10 days, lower titers in <6mos; persist up to 1-3 months ◦ IgG: max in 20-30 days, lower response in <6mos; subclasses IgG1 & 3; booster effect after re-infection with highest level in 5-7 days ◦ IgA Serum IgA: several days after IgG and IgM Freed and cell-bound IgA in nasopharyngeal secretions; free anti-RSV IgA appears 2-5 days after infection and peaks 8-14 days Greater response in >6 months Primary & secondary infection with group-A can induce cross-reactive to group-B Antibody responses to the F protein are cross reactive with both strains, whereas with G protein, the response is subgroup specific RSV: Immune Response • RSV specific IgE: cell bound to the mucosal epithilial of the respiratory tract, not much free detected in the secretions • Amount, persistency and duration are critical in determining the severity of the disease (bronchiolitis and wheezing) RSV: Immune Response • Cell-mediated: CD4+ & CD8+ cells and Th1 and Th2 types of CD4+ • IgE + mast cells inflammatory mediators release • RSV + epithelium mediators release to mobilize other cells – Leukotrienes, eosinophil degranulation byproducts – Epithelial cell-derived cytokines & chemokines – Cell adhesion molecules and homing ligants (CD11B, ICAM-1, Eselectin) mobilize inflammatory and immune cells to the site, to rollover, bind and stick to the virus-infected tissues – Expression of antigen-presenting molecules (HLA class I & II) Wright, M and Peidimone, G. RSV Prevention and Therapy: Past. Present and Future. Ped Pulm. RSV: Manifestations • Severity of illness depending on age, co-morbidities, environmental exposure & h/o previous infection • 2-4 days URI LRTI with cough, wheeze, increased WOB, cyanosis • CXR: patchy infiltration/atlectasis, hyperinflation, & peribronchial thickening • Apnea: 20% in <6mos hospitalized patients – Highest incidence in premies and <1mos – Self-limited, does not recur with subsequent infection – Prolongs reflex central apnea triggered by peripheral sensorineural stimulation Sabogal et al, Effect of RSV on apnea in weanling rats. Pediatr res 2005 RSV: Co-infection • 165 PICU admissions with RSV bronchiolitis • 42% mechanically intubated patients in PICU with lower airway secretions positive for bacteria • Required longer ventilatory support • WBC, neutrophil & CRP are non-conclusive • Organisms: H. influenza, S. aureus, M. catarrhalis, S. penumoniae, S. pyogens – Rare: Pseudomonas, B. pertussis, K. pneumoniae, E. coli Thornburn, K et al. High incidence of pulmonary bacterila co-infection in children with severe respiratory sysncytial virus (RSV) bronchiolitis. Thorz 2006; 61:611-615 RSV: Treatment • Supportive care: fluid, nutrition and hydration • Oxygen supplementation: non-invasive to CMV, to HFOV to ECMO • Deep nasal suction • CPT: administered to mobilize secretions and recruit atelectatic lungs: not beneficial (Cochrane systemic review) RSV: Pharm. Interventions • Bronchiodilators – Beta-agonists: minimally significant improvement in clinical scores but not likely to be clinically significant. No statistically significant improvement in oxygenation, admission rate or LOS (Gadomski and Basale in Cochrane review). Levoalbuterol may have better anti-inflammatory effect than racemic epi in animal model, no clinical trial – Epinephrine: no benefit in in-patient settings but may produce a modest short-term improvement in out patient – Anticholinergic: not effective in RSV RSV: Pharm. Interventions • Corticosteroids: – Systemic: not statistically significant in clinical scores, respiratory rate, oxygen saturation, admission rate and LOS (Patel et al.; Teeratakulpisarn et al.; Corneli et al.) – Inhaled: No difference in reduction in wheezing, readmission rate, use of systemci corticosteroids or use of bronchiodilators (Cochrane review; Ermers et al.) – Combination: oral dexamethasone + inhaled racemic epi significantly less likely to require hospitalization (Plint AC, et al. and dexamethasone in children with bronchiolitis.. N Engl J med 2009;360:2079-2089) Epinephrine RSV: Pharm. Interventions • Antivirals: – Ribavirin: synthetic nucleoside analog. Inhibits RSV replication in vitro, not in vivo » Expensive, difficult to administer, possibly a teratogen » Controversies in inhaled Ribavirin » Recommended either alone or in combination with anti-RSV antibodies to treate infection in select immunocompromised hosts • Antibiotics: co-infections – 0.2% in all bronchiolitis – 40% in intubated patients – Most common sites of co-infections: UTI, OM RSV: Pharm. Interventions • Recombinant Human Deoxyribonuclease (DNAse) – No demonstrable benefits (Boogaard, R. et al. Recombinant human deoxyribonuclease in infants with RSV bronchiolitis. Chest 2007;131:788-795) • Hypertonic saline – Nebulized HTS could reduced LOS without any adverse effects (ZhangL, et al. Nebulized hypertonic saline solution for acute bronchiolitis in infants. Cochrane Databse Syst Rev 2008:(4):CD006458) – 5% nebulized HTS is safe, superior to current treatment (Khalid A., et al. Nebulized 5% or 3% hypertonic or 0.9% saline for the treating acute bronchiolitis in infants. J Ped:2010) RSV: Pharm. Interventions • Surfactant – Decrease surface tension; protein components (A & D) gthat bind viral and bacterial surface markers and facilitate their immune-mediated elimination. Protein D promote alveolar macrophage production of free radicals – Exogenous surfactant decrease ventilation and PICU LOS, improvement of pulm mechanics and gas exchange (Ventre K. et al. Surfactant therapy for bronchiolitis in critically ill infants. Cochrane Database Syst Rev. 2006:(3):CD005150) RSV: Pharm. Interventions • Heliox – No improvement in ventilation or oxygenation (Liet et al.) • Anti-Leukotrienes – Controversies in using monolukast (leukotrienes antagonist) RSV: Immnunoprophylaxis • RSV Immunoglobulin (RSV-IVIG) – Pooled polyclonal human immunoglobuline, administered monthly – Decreased hospitalization and LOS of high risk infant: premies and CLD – Associated with an increase in surgical morbidity and mortality in infants with CHD – Interfere with immune response to live virus, delayed MMR until 9mths – Disadvantages: » Large volume 15ml’kg, infuse over 4-6 hrs fluid overload » Transfer of blood born pathogens RSV: Immnunoprophylaxis • Palivizumab (Synagis) – Humanized monoclonal IgG1 abs produced by recombinant DNA: >95% human with minimally immunogenic, broadly reactive activity to both subtypes; 15ml/kg IM monthly – Preventing infection of upper respiratory tract but also limiting downward spread – Protection for premies without BPD and acyanotic CHD patients – Also decrease risk of long term wheezing – Titers dropped below protective level after first dose and increase after subsequent dose, still with risk of RSV infection after the first 2 doses – Low level in nasal mucosa doesn’t prevent infection but reduces downward spreading RSV: Immnunoprophylaxis • Motavizumab (Rezied) – Second generation IgG1 monoclonal antibody – 70x higher affinity for the RSV F protein. It inhibits RSV replication in upper respiratory tract and fully humanized – Phase III with 26% reduction in hospitalization compared to palivizumab, 50% reduces in outpatient medical management – Not yet approved by FDA