Kimberlin - Red Book Update - American Academy of Pediatrics
advertisement

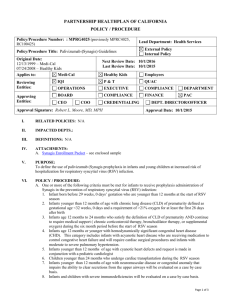
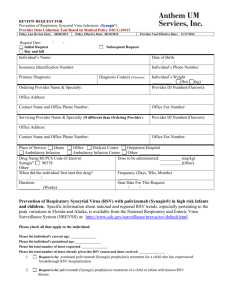
Red Book Update: What To Expect in 2015 David W. Kimberlin, M.D. Editor, Red Book: Report of the Committee on Infectious Diseases Disclosures • I have the following financial relationships with the manufacturer(s) of any commercial product(s) and/or provider of commercial services. – Research Support from: Gilead, GlaxoSmithKline • I do intend to discuss an unapproved/investigative use of a commercial product/device in my presentation. Author: Committee on Infectious Diseases David W. Kimberlin, MD, FAAP, Editor Michael T. Brady, MD, FAAP, Associate Editor Mary Anne Jackson, MD, FAAP, Associate Editor Sarah S. Long, MD, FAAP, Associate Editor AAP Committee on Infectious Diseases (Red Book Committee) • • • • 12 Committee Members (voting) 1 Section on Infectious Diseases Member (voting) 4 Ex Officio Members (Red Book editor and associate editors) 12 Liaisons – – – – – – – – Canadian Paediatric Society (2) CDC (2) National Vaccine Program (2) NIH FDA (2) American Thoracic Society COPAM Pediatric Infectious Diseases Society AAP Committee on Infectious Diseases (Red Book Committee) • Committee members appointed for 6 year terms • Selection influenced by expertise and geography – AAP District and Chapter involvement • Spring and Fall meetings • Committee members serve as liaisons to ACIP Working Groups AAP Committee on Infectious Diseases Red Book Development Process Red Book published every 3 years Work on next edition begins immediately Chapters distributed to primary authors for revision CDC, FDA, and AAP Committees and Sections review • Two designated COID members review • Marathon Meeting in Spring of year prior to publication for discussion of each chapter by full COID • • • • AAP Committee on Infectious Diseases Red Book Development Process • 2015 Edition – – – – – 263 documents (chapters) 150 Primary Reviewers, 62% of whom are new 253 CDC reviewers 68 FDA reviewers 43 AAP Internal Review committees AAP Committee on Infectious Diseases Red Book Development Process • Purpose of the Red Book: – Composite summary of current AAP recommendations representing the policy of the AAP on various aspects of infectious diseases – Recommendations represent a consensus of opinions based on consideration of the best available evidence by members of the COID, in conjunction with liaison representatives from CDC, FDA, NIH, National Vaccine Program Office, Pediatric Infectious Diseases Society, Canadian Paediatric Society, American Thoracic Society, Red Book consultants, and numerous collaborators Respiratory Syncytial Virus Immunoprophylaxis With Palivizumab Viral Bronchiolitis, 2007-2010 2,207 Hospitalized Patients < 2 yoa • • • • • • • • • • RSV Human rhinoviruses Adenoviruses Coronaviruses Human metapneumoviruses Enteroviruses Parainfluenza viruses 1,2,3 Influenza A, B Human bocavirus Co-infection 73% 26% 8% 7% 7% 5% 3% 1% NA 32% Arch Pediatr Adolesc Med 2012:166(8):700 Palivizumab Binding of RSV Fusion Protein AAP Guidance Regarding RSV Immunoprophylaxis • January 1996 • April 1997 RespiGam licensed by FDA AAP Statement: RSV-IVIG Indications • • • • • • • • Palivizumab licensed by FDA AAP Statement: Indications for use of palivizumab AAP Statement: Revised indications for palivizumab Revised indications Revised indications AAP Statement: Revised indications for palivizumab No major changes Updated Guidance for palivizumab prophylaxis* June 1998 November 1998 December 2003 2006 Red Book 2009 Red Book December 2009 2012 Red Book August 2014 * Pediatrics 2014:134(2):415-420 Pediatrics 2014:134(2):e620-e638 Rationale for Revisions to AAP Guidance • • • • • • • • • • • Data on seasonality of RSV circulation Data showing risk of RSV hospitalization by gestational age Data regarding palivizumab pharmacokinetics Data showing a decline in incidence of bronchiolitis hospitalizations Data showing no difference in RSV hospitalization rates or RSV attack rates between African-American and white children <24 m of age Data showing mortality rates among children hospitalized with RSV are lower than previously estimated Data showing a statistically significant but clinically limited impact on episodes of wheezing Reports indicating little benefit from prophylaxis among children with Down syndrome and cystic fibrosis Reports describing palivizumab resistant RSV isolates among children hospitalized with breakthrough RSV infection Independently conducted cost-analyses demonstrating high cost versus limited benefit Need to simplify guidance Goals of AAP Recommendations • Target infants at highest risk for severe disease with risk factors that are most consistent and predictive • Optimize balance of benefit and cost • Simplify approach for providers Participants in 2014 AAP Guidance Revisions • AAP Bronchiolitis Guidelines Committee • AAP Committee on Infectious Diseases • 21 Committees, Councils, Sections, and Advisory Groups within the AAP • Outside Groups – – – – – – American Academy of Family physicians American College of Chest Physicians American College of Emergency Physicians American Thoracic Society Emergency Nurses Association Society of Hospital Medicine • Data presented to AAP by the manufacturer Preterm Infants Without Chronic Lung Disease • Updated guidance – In the first year of life, palivizumab prophylaxis is recommended for infants born before 29 weeks 0 days gestation – Palivizumab prophylaxis is not recommended for otherwise healthy infants born at or after 29 weeks 0 days gestation • Previous guidance – Previously, prophylaxis was recommended for infants with preterm birth before 32 weeks gestation. Infants with certain risk factors born between 32 weeks 0 days through 34 weeks 6 days were eligible. RSV Hospitalizations Among Children < 24 Months of Age Pediatrics 2013;132:e341 Hall et al, Pediatrics 2013:132(2):e341-e348 Average RSV Hospitalization Rates For Children < 24 months (2000-2005) Children < 24 months N Rates of RSV Hospitalization/1,000 95% CI All infants regardless of gestational age 559 5.2 4.8-5.7 All term infants (≥ 37 week) 479 5.3 4.9-5.8 All preterm infants (< 37 wk) 56 4.6 3.4-5.8 ≥ 35 week gestation 494 5.1 4.7-5.5 32-34 week gestation 23 6.9 4.3-10.1 29-31 week gestation 6 6.3 2.0-12.4 < 29 week gestation 12 19.3 8.4-34.0 All very preterm (< 30 week) 15 18.7 10.0-30.0 Hall et al, Pediatrics 2013:132(2):e341-e348 RSV Hospitalizations Among 1,029 Infants Born ≤ 32 Weeks Gestation Gestational Age (weeks) # of Infants # of RSV % Admissions Admitted P-value versus 30-32 Weeks’ Gestation ≤ 26 165 23 13.9 <.001 27-28 > 28-30 171 240 17 18 9.9 7.5 .007 .12 > 30-32 453 20 4.4 Comparator Total 1029 78 7.6 Not Applicable Stevens et al, Arch Pediatr Adolesc Med 2000;154:55-61 RSV Hospitalization for Children < 24 Months by Gender and Race, 2000–2005 No difference in hospitalizations rates by race within first 6 months of life Hall et al, Pediatrics 2013:132(2):e341-e348 No Difference in Rates of RSV Hospitalization Between African-American and White Children Striped bars: Black children 0 to 5 months Dashed bars: White children 0 to 5 months Black bars: Black children 6 to 59 months White bars: White children 6 to 59 months Iwane et al, Am J Epidemiol 2013:177(7):656-665 RSV Hospitalizations/1,000 Children from > 248,000 Child-Years of Follow-up Age/Risk Group 0 to <6 months 6 to <12 months 12 to 24 months IRR (95% CI) for 0 to <6 months Low risk infants 44.1 15.0 3.7 comparator Infants with CHD 120.8 63.5 18.2 2.7 (2.2-3.4) Infants with CLD 562.5 214.3 73.4 12.8 (9.3-17.2) ≤28 week gestation 93.8 46.1 30.0 2.1 (1.4-3.1) 29 to <33 week gestation 81.8 50.0 8.4 1.9 (.4-2.4) 33 to <36 week gestation 79.8 34.5 10.8 2.8 (2.1-3.1) Boyce et al, J Pediatr 2000:137(6):865-870 Preterm Infants With Chronic Lung Disease • Updated guidance – In the first year of life, palivizumab prophylaxis is recommended for preterm infants with chronic lung disease of prematurity defined as < 32 weeks, 0 days' gestation and a requirement for > 21% oxygen for at least 28 days after birth • Previous guidance – Previously no definition of chronic lung disease was provided. Infants With Congenital Heart Disease • Updated guidance – Clinicians may administer palivizumab prophylaxis in the first year of life to infants with acyanotic, hemodynamically significant heart disease. – Consultation with a cardiologist is recommended for patients with cyanotic heart disease for decisions about prophylaxis. • Previous guidance – Previously prophylaxis was recommended in the second year of life for this cohort. Palivizumab Cardiac Study Incidence of RSV Hospitalization Absolute Percent Reduction 4.4% Placebo n=648 9.7% n=63 Palivizumab n=639 5.3% n=34 Cyanotic group 7.9% n=27 5.6% n=19 2.3% 0.285 Acyanotic group 11.8% n=36 5.0% n=15 6.8% 0.003 Primary analysis: p-value 0.003 Feltes et al, J Pediatr 2003:143(4):532-540 Number of Monthly Doses • Updated guidance – Clinicians may administer up to a maximum of 5 monthly doses of palivizumab during the RSV season to infants who qualify for prophylaxis in the first year of life (including Florida). Qualifying infants born during the RSV season will require fewer doses. For example, infants born in January would receive their last dose in March. – Maximum 5 monthly doses for all states • Previous guidance – Previously, fewer than 5 monthly doses were recommended for some infants Simulated Palivizumab Concentration-Time Profiles 40µg/mL Robbie et al, Antimicrob Agents Chemother 2012:56(9):4927-4936