Immunoprphylaxis for Prevention of Severe respiratory Syncytial
advertisement
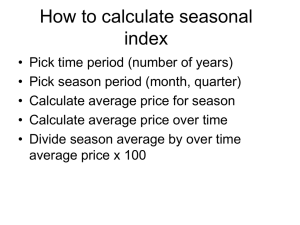
Immunoprophylaxis for Prevention of Severe RSV Bronchiolitis Ma. Teresa C. Ambat, MD Neonatology-TTUHSC 11/21/2008 Development of Immunoprophylaxis 1996: FDA approved the intravenous polyclonal antibody RSV immune globulin (RSV-IVIG, Respigam) Prepared from donors selected for high serum titers of RSV neutralizing antibody No longer available 1998: FDA approved palivizumab (Synagis) First monoclonal antibody developed into vaccine, for use as immunoprophylaxis for children <2 yrs at risk for severe RSV infection Comparison of RSV-IVIG with Palivizumab Characteristics RSV-IVIG (Respigam) Palivizumab (Synagis) Type of immunoglobulin Polyclonal Monoclonal Method of administration IV IM Contraindicated in infants with hemodynamically significant CHD Yes No Protects against other viral infections Yes No Decreased AOM Yes No Risk of fluid overload in BPD Yes No Blood product Yes No Interferes with routine childhood immunization Yes No 750mg/k/dose 15mg/k/g/dose Monthly Monthly 5 5 Dosage Dosing interval # of doses / season Clinical Practice Guideline Diagnosis and Management of Bronchiolitis RECOMMENDATION 8a Clinicians may administer palivizumab prophylaxis to selected infants and children with CLD or a history of prematurity less than 35 weeks’ gestation or with congenital heart disease Recommendation: evidence level A; RCT; preponderance of benefit over harm Clinical Practice Guideline Diagnosis and Management of Bronchiolitis RECOMMENDATION 8b When given, prophylaxis with palivizumab should be given in 5 monthly doses, usually beginning in November or December, at a dose of 15 mg/kg per dose administered intramuscularly Recommendation: evidence level C; observational studies and expert opinion; preponderance of benefit over cost The 2006 Red Book Recommendations for the use of Palivizumab 1. Palivizumab prophylaxis should be considered for infants and children < 24 months of age with chronic lung disease of prematurity who have required medical therapy (supplemental oxygen, bronchodilator or diuretic or corticosteroid therapy) for CLD within 6 months before the start of the RSV season. Patients with more severe CLD who continue to require medical therapy may benefit from prophylaxis during a second RSV season. Data are limited regarding the effectiveness of palivizumab during the second year of life. The 2006 Red Book Recommendations for the use of Palivizumab 2. Infants born at 32 weeks of gestation or earlier may benefit from RSV prophylaxis, even if they do not have CLD. Major risk factors: gestational age, chronologic age at the start of the RSV season < 28 weeks of gestation or earlier may benefit from prophylaxis during their first RSV season, whenever that occurs during the first 12 months of life 29 to 32 weeks of gestation may benefit most from prophylaxis up to 6 months of age Once a child qualifies for initiation of prophylaxis at the start of the RSV season, administration should continue throughout the season and not stop at the point an infant reaches either 6 months or 12 months of age. The 2006 Red Book Recommendations for the use of Palivizumab 3. Prophylaxis should be considered for infants between 32 and 35 weeks of gestation younger than 6 months of age at the start of RSV season only if 2 or more of these risk factors are present: Child care attendance School-aged siblings Exposure to environmental air pollutants Congenital abnormalities of the airways Severe neuromuscular disease No single risk factor causes a very large increase in the rate of hospitalization, and the risk is additive as the number of risk factors for an individual infant increases. The 2006 Red Book Recommendations for the use of Palivizumab 4. Results from clinical trials indicate that palivizumab trough serum concentrations 30 days after the fifth dose will be well above the protective concentration for most infants. If the first dose is administered in November, 5 monthly doses of palivizumab will provide substantially more than 20 weeks of protective serum antibody concentrations for most of the RSV season, even with variation in season onset and end. The 2006 Red Book Recommendations for the use of Palivizumab 5. Children who are 24 months of age or younger with hemodynamically significant cyanotic and acyanotic congenital heart disease will benefit from palivizumab prophylaxis. Children younger than 24 months of age with congenital heart disease who are most likely to benefit from immunoprophylaxis include: Infants who are receiving medication to control congestive heart failure Infants with moderate to severe pulmonary hypertension Infants with cyanotic heart disease Summary of AAP Recommendations for Use of Immunoprophylaxis in RSV Infection 1. 2. 3. Without BPD With BPD Former Premature Infants Irrespective of Prematurity GA <28 wks, who are <12 months old at the start of RSV season GA >28 to <32 wks, who are < 6 months old at the start of RSV season GA >32 to <35 wks, who are <6 months old at the start of RSV season and > 2 of the ffg: Child care attendance School-aged siblings Congenital anomalies of the airways Severe neuromuscular disease Exposure to environmental air pollutants 1. 2. <12 months old at the start of the 1st RSV season <24 months old with persistent signs of BPD at the start of the 2nd RSV season Summary of AAP Recommendations for Use of Immunoprophylaxis in RSV Infection 1. Infants and children with congenital heart disease At the start of RSV season <12 months and receiving medications to control CHF <12 months with uncorrected or partially corrected cyanotic heart disease who remain cyanotic <24 months with hemodynamically significant cyanotic and acyanotic heart disease 2. Infants and children with pulmonary hypertension At the start of RSV season <12 months with moderate PPHN <24 months with severe PPHN Summary of AAP Recommendations for Use of Immunoprophylaxis in RSV Infection Dates for initiation and termination should be based on the same considerations as for high-risk preterm infants. For children who underwent cardiopulmonary bypass and still require prophylaxis, a postoperative dose of palivizumab (15mg/kg) should be considered as soon as the patient is hemodynamically stable. Summary of AAP Recommendations for Use of Immunoprophylaxis in RSV Infection 3. Infants and children not considered at risk for severe RSV (immunoprophylax is not indicated) Infants with non-hemodynamically significant heart disease: ASD Small VSD, Pulmonic stenosis, mild coarctation, PDA Infants with corrected cardiac lesions without cyanosis or CHF Infants with mild cardiomyopathy who are not receiving medical therapy Additional AAP Remarks Once a child qualifies for immunoprophylaxis, administration should continue for the remainder of the RSV season even if the child no longer meets the clinical criteria or age requirement prior to completion of the RSV season. Even if a child develops RSV during immunoprophylaxis, he or she should complete the drug course. Neither RSV-IVIG nor Palivizumab is indicated or licensed for the treatment of RSV infection. RSV prophylaxis should begin before the onset of the RSV season (November) and terminate at the end of the RSV season (March), allowing for 6 months of protection. Additional AAP Remarks All high-risk infants and their contacts should be immunized against influenza beginning at age 6 months. There is insufficient information regarding the immunoprophylaxis of infants with CF, SCID, AIDS. However, they may benefit from prophylaxis. There are no recommendations regarding the administration of palivizumab as a means of preventing nosocomial RSV infection. Additional AAP Remarks High-risk infants should never be exposed to tobacco smoke. Existing data are conflicting regarding the specific protective effect of breastfeeding against RSV infection. High-risk infants should be kept away from crowds and from situations in which exposure to infected individuals cannot be controlled. Participation in group child care should be restricted during the RSV season for high-risk infants whenever feasible. Parents should be instructed on the importance of careful hand hygiene. Controversies in RSV Immunoprophylaxis Primary benefit of RSV immunoprophylaxis is decreased rate of RSV-related hospitalizations. No significant decrease in rate of mortality attributable to RSV infection in infants who received prophylaxis. Most of the economic analyses fail to demonstrate overall savings in health care dollars because of the high cost if all atrisk children were to receive prophylaxis. Giving immunoprophylaxis to all infants at high risk is not cost effective. References 1. 2006 Redbook 2. Clinical Practice Guideline: Diagnosis and Management of Bronchiolitis. Endorsed by the American Academy of Family Physicians, the American College of Chest Physicians, and the American Thoracic Society. 3. Brodsky D, Quellette M. Primary Care of the Premature Infant. 2008.