Repro18-MaleHistoI
advertisement

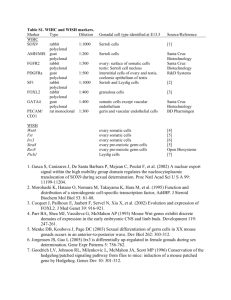
Repro #18 Tue 04/01/03 10am Dr. Cammarata M. Messa Proscribe Samera Kasim Page 1 of 5 Male Histo I Look at several different slides of this information. For example, Sertoli cells can vary widely. Several slides were shown demonstrating this. Also remember that color varies depending on the stain. The Color atlas has pictures that represent those which were shown in class relatively well. I. The Testis A. Introduction 1. The testis is suspended within the scrotum and is immediately surrounded by the testicular capsule, composed of 3 layers a) the outer component, the tunica vaginalis is a single layer of mesothelial cells frequently destroyed by preparation; allows testis to move in scrotum b) the middle layer is the most prominent and is the tunica albuginea (i) thick layer of dense fibro-elastic connective tissue with scattered smooth muscle c) innermost layer of the testicular capsule is the tunica vasculosa (i) network of blood vessels embedded within a delicate areolar connective tissue 2. The tunica albuginea is thickened along the posterior surface of the testis where it projects into the gland as the mediastinum testis 3. Thin C.T. partitions, testicular septa extend radially from the mediastinum testis to the capsule dividing the interior of the testis into 250 pyramidal compartments of lobuli testis a) apex of each lobule directed towards the mediastinum b) each lobule contain 1-4 highly convoluted seminiferous tubules c) each S.T. is embedded in a loose connective tissue stroma containing vessels, nerves, and interstitial cells of Leydig d) each ST starts and stops at the same point without leaving the testis 4. the testis are a hormonal gland; they produce testosterone 5. they’re also responsible for procreation. 6. the tunica vascularis is a layer sometimes mentioned by textbooks; it’s the inner layer of the tunica albuginea and contains blood vessels. B. Seminiferous Tubules (ST) 1. Introduction a) each lobule of the lobuli testis is composed of 1-4 highly convoluted seminiferous tubules b) each seminiferous tubule is highly convoluted and is about 0.2 mm in diameter and 30 to 70 cm long c) at the apex of a lobule each tubule loses its convolutions and becomes a straight tubule (aka tubuli recti) d) these have a thick basal lamina Repro #18 Tue 04/01/03 10am Dr. Cammarata M. Messa Proscribe Samera Kasim Page 2 of 5 Overview: Moving from out to in (basal lamina lumen): germ line cells mature and migrate toward the lumen, making distinct changes, until eventually the sperm is released in the lumen of the S.T. Seminiferous Epithelium a) the tubules are lined by a complex germinal epithelium which is stratified b) composed of two major cell types: supporting cells and spermatogenic cells c) seminiferous epithelium rests on a basal lamina with peritubular tissue externally Sertoli Cells a) columnar cell population sitting on a basal lamina and extending through the full thickness of the epithelium to the free surface, 70-90 microns b) a fixed population of non-proliferating support cells c) spermatogenic cells occupy deep recesses in the lateral and apical surfaces d) morphology (i) oval nucleus with a distinct nucleolus (ii) a well established smooth endoplasmic reticulum system with numerous lysosomes and a distinct Golgi system (iii) tight junctions at the base of adjacent Sertoli cells participate in the formation of a blood-testis barrier (iv) on slides, mostly nucleus is visible. The nucleus can be many shapes. (v) The cells are VERY tall columnar, although they may not look like it because the lateral borders are so difficult to see. They are complex and bound with many “things.” (vi) Look for the prominent nucleus when looking for Sertoli cells e) other aspects include: (i) resistant to heat, ionizing radiation and some toxic agents (a) this is important because they don’t reproduce (ii) blood-testis barrier (a) the body can make Ab against their own germ line. That’s why it’s important that this barrier exists. (iii) support and provide nutrition of the germ cells (iv) mediate movement of spermatogenic cells from basal lamina to lumen (a) they’re in close juxtaposition to germ cells (v) release late spermatids into tubule lumen (vi) phagocytize residula cytoplasm after release of late spermatids, as well as degenerative germ cells (vii) secretes fluids, including androgen binding protein and inhibin e) 2. 3. Repro #18 Tue 04/01/03 10am Dr. Cammarata M. Messa Proscribe Samera Kasim Page 3 of 5 (viii) 4. receptor mediated binding of FSH and testosterone (a) they contain the receptor for FSH (b) also, high levels of testosterone are needed for germ line differentiation. (ix) also divides the Basal department from the Adlumenal department (a) the basal department houses the undifferentiated cells, while the adlumenal contains stem cells that are undergoing differentiation. Germ Cells: a proliferative population that migrates continuously from the periphery of the tubule to the luminal free surface a) cells include: spermatogonia, spermatocytes and immature and mature spermatids b) process is called spermatogenesis (also see diagram) c) spermatogonia: two types (e.g. A and B) have been described (i) spermatogonia are about 12 um in diameter and border the basal lamina of the seminiferous tubule (ii) nuclei are round/ovoid with nucleoli while cytoplasm stains lightly (iii) some spermatogonia (A) serve as stem cells and undergo mitosis slowly while others (B) are committed to the production of spermatocytes (a) there are 3 types of spermatogonia: (i) B cells (ii) Pale A cells (iii)Dark A cells (b) Pale type A cells divide to form pale A and B spermatogonia (c) Dark type A normally don’t divide, but if they do, they make pale A cells (d) Type B divide via mitosis to form diploid primary spermatocytes. (i) B cells sit on the basal lamina (“basal cells”) d) spermatocytes: both primary and secondary are present (i) primary spermatocytes are the largest germ cells and concentrate in the middle zone of the epithelium (Meiosis) (ii) secondary spermatocytes are about half the volume and lie closer to the lumen (somatic mitosis) (a) You will not need to be able to decipher between primary and secondary spermatocytes on the slides (b) Remember that genetic exchange occurs e) spermatids arise from secondary spermatocytes (the second meiotic event) (i) lie close to lumen Repro #18 Tue 04/01/03 10am Dr. Cammarata M. Messa Proscribe Samera Kasim Page 4 of 5 (ii) no further divisions but spermiogenesis transforms spermatid into a spermatozoa (iii) spermatids are NON motile (iv) there are early and late spermatids; they are not fully mature until in the epididymus where they become motile. (v) these are the haploid cells (vi) on slides, the nuclei look more solid compared to spermatocytes, which are grainy because of the active chromatin (vii) there was a class demonstration that showed the differentiation of the male germ line. Make sure you understand each meiotic event, the number of chromosomes present at each step and whether the cell is diploid or haploid… (viii) Also know that 1 basal cell gives rise to 4 haploid spermatids (ix) See graphic 18.2 in color atlas; there is a lot of mitochondria seen in the cross-section of the middle piece. Less is seen in the principle cross-section. I would be familiar w/ this figure. C. Peritubular tissue 1. This tissue contains numerous connective tissue fibers, flattened fibroblasts and some smooth muscle cells (myoid cells) a) smooth muscle may aid in the movement of spermatozoa along the length of the tubule b) tends to increase with age and be extensive in certain cases of infertility 2. Blood vessels and nerves enter and leave from the mediastinum and form networks around the tubules 3. Interstitial cells of Leydig are a marked feature of this tissue a) source of the male sex steroid hormone, testosterone b) they lie in compact groups, usually in the angular areas created by the seminiferous tubules c) large vacuolated cells, with distinct nucleus with a distinct nucleolus. Binucleate cells are common d) extensive development of smooth endoplasmic reticulum. (i.e. steroid synthesis) e) on the slides, look between the basal lamina outside the seminiferous tubules. f) They stain lightly g) Usually found in clusters D. Hormonal control of male reproductive function 1. The structure and endocrine function of the interstitial cells are controlled by LH. 2. Testosterone is required to maintain spermatogenesis. It therefore, exerts a positive control on Sertoli (and germ) cells. Excessive testosterone acts as a feedback inhibitor to regulate LH production and secretion by acting on the pituitary gland and hypothalamus. Repro #18 Tue 04/01/03 10am Dr. Cammarata M. Messa Proscribe Samera Kasim Page 5 of 5 3. 4. 5. 6. 7. 8. The primary target cell for FSH is the Sertoli cell, stimulating protein synthesis Sertoli cells respond to FSH by secreting androgen binding protein which binds to testosterone Inhibin is a feedback inhibitor which regulates FSH secretion from the pituitary gland. FSH (and LH) are released from the gonadotrophic cells in the adenohypophysis of the pituitary gonadotrophic cells in the hypothalamus are responsible for stimuluating production of the releasing factor in the pituitary it is hypothesized that Sertoli cells may feedback to leydig cells to control secretions KNOW THIS: Below is an explanation that Dr. Cammarata sat down and gave me regarding the Mitotic and Meiotic events of B cells spermatids. “THERE WILL BE A QUESTION OVER THIS ON THE TEST.” A cells differentiate into A and B cells. You cannot tell these two types of cells apart on a slide. B cells (basal cells) are stem cells. They have 46 chromosomes. B cells undergo mitosis to become primary spermatocytes. They also have 46 chromosomes (because during mitosis, genetic material is duplicated) and are tetrad (4N) in DNA. This is the only mitotic event. The rest are meiotic The first meiotic event: primary spermatocytes undergo meiosis to become secondary spermatocytes. This process lasts 16 days, aka a long time! Thus there are more primaries than secondaries. You cannot determine the difference between primary and secondary on a slide. Secondary spermatocytes have 23 chromosomes and are 2N (diploid) in their DNA. The second meiotic event: secondary spermatocytes undergo a meiotic event to become spermatids. This last ONLY 8-16 hours. (early) Spermatids have 23 chromosomes and are 1N (haploid) in their DNA. Early Spermatids undergo maturation, eventually becoming a late spermatid. During this process, there is no further division and reduction of chromosome/DNA. (ie. This is NOT mitosis or meiosis) Be prepared to answer questions as follows: If an arrow is pointing to a cell on a slide, be able to identify the cell, determine the number of chromosomes, and how much DNA is present. Know the length of time of each division