Ch 12- Forensic Serology - Bio-Guru
advertisement

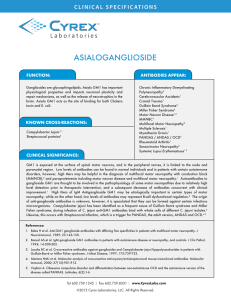
Forensic Serology Chapter 12 Karl Landsteiner In 1901 he discovered that all humans do not have the same blood type He discovered the A-B-O blood group system This saved millions of lives by preventing mismatched blood transfusions Other researchers were able to discover the Rh factor because of his research 29 years later, they gave Karl a Nobel Prize Other Blood Factors The ABO proteins and Rh factor proteins are not the only proteins on the surface of blood cells There are more than a 100 different surface blood factors But the ABO factors are most important for matching a donor to a recipient Blood and Forensics No 2 individuals (except identical twins) can share all the 100+ blood factors So forensic scientists used this tool to link blood from a crime scene to an individual After 1990 however, DNA fingerprinting has been used instead of blood typing to identify blood stains and other biological evidence. What is Blood? Various cell types found in a liquid matrix called plasma • Erythrocytes (RBCs) – Transport O2, CO2 – Stay within blood vessels • Leukocytes (WBCs) – Fight infection (immune system) – Can move from blood vessels into tissues • Platelets (Cell fragments) – Help with clotting White Blood Cell Platelets Red Blood Cells Characteristics of Red Blood Cells Red blood cells (erythrocytes) are biconcave disks that contain oxygen-carrying hemoglobin. Red blood cells discard their nuclei, mitochondria and most organelles during development and so cannot reproduce or produce proteins. In addition to 100s of cell surface proteins, their cell surfaces have a special class of blood factor proteins called Antigens. There are at least 15 different antigens, but the most important are the ABO and Rh antigens Role of RBCs Transport inhaled O2 from lungs to all body cells Remove CO2 from all body cells and take it back to lungs for exhalation When oxygen combines with hemoglobin bright red oxyhemoglobin results. Deoxygenated blood or blood containing CO2 (deoxyhemoglbin) is darker. RBCs are destroyed after about 120 days Summary of Functions of WBCs Leukocytes can squeeze between cells lining walls of blood vessels by diapedesis and attack bacteria and debris. Neutrophils and monocytes are phagocytic, with monocytes engulfing the larger particles. Eosinophils moderate allergic reactions as well as defend against parasitic infections. Basophils migrate to damaged tissues and release histamine to promote inflammation and heparin to inhibit blood clotting. Lymphocytes are the major players in specific immune reactions and some produce antibodies (T cells and B cells) Blood Platelets Blood platelets are fragments of cells Platelets help repair damaged blood vessels by adhering to their broken edges. Thrombopenia, or low platelet counts increase bleeding risks Thrombocytosis or high platelet count may lead to thrombosis (clotting, bruising, strokes, heart attacks). Blood Plasma • Plasma is the clear, straw-colored fluid portion of the blood. • Plasma is mostly water, with a mixture of, amino acids, proteins, carbohydrates, lipids, vitamins, hormones, electrolytes, and cellular wastes Hematocrit Hematocrit means the percentage of red blood cells in blood A blood hematocrit is normally 45% cells and 55% plasma. Buffy Coat? Buffy coat is the layer that contains most of the white blood cells and platelets. “Buffy” because it is buff (color of naked skin) in color The buffy coat is used to extract DNA from blood - RBCs have no DNA, only WBCs do. ABO Blood Group Type A blood has A antigens on red blood cells and antiB antibodies in the plasma. Type B blood has B antigens on red blood cells and antiA antibodies in the plasma. Type AB blood has both A and B antigens, but no antibodies in the plasma. Type O blood has neither antigen, but both types of antibodies in the plasma. Adverse transfusion reactions are avoided by preventing the mixing of blood that contains matching antigens and antibodies. – Adverse reactions are due to the agglutination of red blood cells. Rh Blood Group The Rh factor was named after the rhesus monkey. If the Rh factor surface protein is present on red blood cells, the blood is Rh positive; otherwise it is Rh negative. There are no corresponding antibodies in the plasma unless a person with Rh-negative blood is transfused with Rh-positive blood; the person will only then develop antibodies for the Rh factor. Blood Groups and Transfusions Antigens and Antibodies Clumping of red blood cells following transfusion is called agglutination. Agglutination is due to the interaction of proteins on the surfaces of red blood cells (antigens) with certain antibodies carried in the plasma. Only a few of the antigens on red blood cells produce transfusion reactions. – These include the ABO group and Rh group. Agglutination of RBCs Antibody: a protein that destroys or inactivates a specific protein antigen. Antibodies are found in the blood serum Antibodies are very SPECIFIC to an antigen. They are designed by the immune system to fit an antigen. Antiserum: blood serum in which there are specific antibodies Agglutination: the clumping together of red blood cells by the action of an antibody Precipitin: an antibody that reacts with its corresponding antigen to form a precipitate Secretor: an individual who secretes his or her bloodtype antigen(s) in body fluids. Approximately 80 percent of the population are secretors Enzyme: a type of protein that acts as a catalyst for certain specific reactions Iso-enzymes: multiple molecular forms of an enzyme, each having the same or very similar enzyme activities Antibodies or Agglutinins Proteins that are present in the serum responsible for ensuring that the only blood cells that can survive in a person are cells of the correct blood type Type O Blood Possessed by people whose genotype is OO both parents passed on the O gene have no antigens these cells can be introduced into a person with Type A or Type B because these cells are not attacked by the antibodies these people possess have both a & b antibodies can only have other O type cells mixed with this blood Relative Frequency of Blood Types in Human Populations Population US whites US blacks Chinese Eskimos Armenians Bolivian Indians O .453 .491 .439 .472 .298 .931 A .413 .265 .270 .452 .499 .053 B .099 .201 .233 .059 .132 .016 AB .035 .043 .058 .017 .080 .001 DRUG - DETECTION Hypothesis: Since foreign substances in blood are identified and then isolated by the immune system, it should be able to detect the presence of drugs and other chemicals. This hypothesis is incorrect. The immune system only creates antibodies and launches attacks against foreign proteins (either free proteins or ones bound to cells) and not against other chemical compounds. We can fool the immune system The drug can be attached to a carrier molecule that is a protein This drug-protein combo can be injected into an animal such as a rabbit or rat (no human volunteers) The animal’s immune system will create antibodies that are specific to the shape of this drug-protein combo molecule We can isolate these antibodies from the animal’s blood serum And use these antibodies to detect the presence of the drug in human blood or urine Polyclonal Antibodies Usually when the immune system produces antibodies, they are a mixture of immunoglobulin molecules designed to recognize and bind to many different sites on an antigen molecule or different epitopes. In other words, they are made against a specific antigen, but each recognizing a different epitope on the antigen. These antibodies are called Polyclonal antibodies Polyclonal antibodies are not very specific or reliable Because the animal makes so many different kinds for ONE antigen, the antibodies may not be consistent and some antibody molecules may not work very well. Monoclonal Antibodies Monoclonal antibodies are those that are not only specific to one antigen, but specific an exact epitope on that antigen. In other words, it is a collection of identical antibodies that bind to a single antigen site or epitope. How are polyclonal antibodies made? 1. Inject the animal with the protein (antigen) and wait for a period of time for the animal to make polyclonal antibodies 2. Then collect the animal’s serum which will contain the polyclonal antibodies. How are monoclonal antibodies made? 1. Inject the animal with the protein (antigen) 2. Remove the spleen and isolate spleen cells (the spleen produces the antibodies) 3. Fuse the antibody-producing spleen cells with tumor cells that were already growing in culture (these are now called hybridoma cells) 4. Grow the hybridoma cells in culture and isolate the cells that are producing the antibody of your choice. 5. These cells will be making antibodies that bind to only ONE epitope on the antigen. The cells can be maintained indefinitely. 6. The antibodies are therefore called monoclonal antibodies. Now how does a criminalist use these monoclonal antibodies? To detect drug presence in blood, urine, etc. A.K.A. EMIT assays (bio jargon for test) EMIT stands for Enzyme-multiplied Immunoassay Technique EMIT is most often used to test for marijuana (THC) metabolites in urine. One of the primary THC metabolites is THC9-carboxylic acid How EMIT works Let’s suppose you’re checking someone’s urine for the presence of THC-9-carboxylic acid (from THC or Marijuana.) 1. 2. 3. 4. 5. 6. Take urine sample to be tested Add monoclonal antibodies for THC-9-carboxylic acid to the urine The antibodies will immediately bind to any THC-9carboxylic acid molecules present in the urine Then add enzyme-labeled THC-9-carboxylic acid molecules to the urine Any antibodies that did not bind to THC-9-carboxylic acid prior to this step (extra antibody molecules), will bind to the enzyme-labeled THC-9-carboxylic acid One can now measure the amount of unbound or unused enzyme-labeled THC-9-carboxylic acid to get a value of THC originally present in the urine. Questions for a Criminalist: 1. 2. 3. Is it blood? Is it human blood? If it is human, can it be linked to a suspect / victim and how closely? Color tests to identify human blood The Benzidine color test was used for years to identify human blood But benzidine was identified as a carcinogen, so nowadays the phenolphthalein test is performed instead. The phenolphthalein test is also known as the Kastle-Meyer color test Both, the benzidine and the Kastle-Meyer test look for the presence of hemoglobin in the sample. The Kastle-Meyer Test When blood, phenolphthalein and hydrogen peroxide are mixed, the hemoglobin in the blood will cause the normally colorless phenolphthalein to a bright pink color This test can yield some false positives Certain vegetable matter can produce the bright pink positive (such as potatoes) Death By Potato? Although the KastleMeyer test can give a false positive in the presence of certain plant matter, it is unlikely that this plant matter would be present at a crime scene and be mistaken for blood. Other blood detection tests Doctors use Hemastix© strips to detect blood in urine But these strips can be used at a crime scene to detect fresh or dried blood. One simply moistens them with distilled water and wipes the bloodstain A color change to green is a positive indicator of blood Bayer Hemastix© Luminol Luminol is a chemical that exhibits chemiluminescence, with a striking blue glow, when mixed with an appropriate oxidizing agent. It is a white to slightly yellow crystalline solid that is soluble in water and most polar organic solvents. Usually, a solution of hydrogen peroxide (H2O2) and a hydroxide in water is used as the activator. In the presence of a catalyst such as an iron compound, the hydrogen peroxide is decomposed to form oxygen and water: What do you see with luminol? It glows a bright blue in the dark, when it comes in contact with bloo Advantages of using Luminol Allows one to detect stains that would not be ordinarily be visible Extremely sensitive - can use it in very dilute concentrations This allows the CSI to spray large areas with it It does not interfere with DNA, so a CSI can collect samples for DNA analysis even after it was sprayed with luminol. Bloody Footprints that were wiped Drawbacks Luminol glows even in the presence of certain other fluids – semen, feces, bleach, tonic water, etc. Luminol glows in the presence of certain vegetable matter - Mr. Potato head strikes again! Thanks to Quinine Crystal Tests Less sensitive than color tests They involve the crystallization of certain components of blood when certain chemicals are added Takayama test and Teichman test Not used as much by CSI So we know it’s blood – but is it human? The Precipitin Test – Rabbits injected with human blood – They make antibodies in their serum – They are bled and the serum recovered – The serum is called human antiserum, because it will react to human antigens – It will cause coagulation when mixed with human blood Precipitin Test (Human blood) (Human antiserum made in rabbits) Gel Diffusion Test Antigen (blood) and antibodies (human antiserum from rabbits) are placed in separate wells in a gel. They are forced to move towards each other. If they bind to each other, they form a single line of precipitate in between the wells This is a positive for human blood DNA TEST DNA testing is the ultimate It has made most other tests for determining if the blood is human, obsolete Analyzing Bloodstain Patterns 1. Surface Texture – 2. Direction of travel – 3. – 4. The harder and less porous the a surface, the less spatter results The pointed end of a bloodstain always faces the direction of travel Impact angle If the strike angle is 90deg then the stain is circular. As the strike angle increases, the stain becomes more and more elongated Origin of blood spatter – If you draw straight lines through the long axis of several blood stains, the point where the lines converge is the origin of the blood spatter Types of Blood Stain Patterns 1. 2. 3. Passive Projected Transfer 1. Passive Bloodstains Passive stains are drops created or formed by the force of gravity acting alone. This category can be further subdivided to include: Drops Drips Pools Passive drops on various surfaces • Blood droplets that strike a hard smooth surface, like a piece of glass, will have little or no distortion around the edge. • Blood droplets that strike a rough surface have a slightly different appearance. They tend to be distorted, scalloped or spined at the edges. Passive: Dripped Blood patterns created by a volume of blood, from same source to target distance (repeated drops onto same spot.) 2. Projected Bloodstains • Projected bloodstains are created when an exposed blood source is subjected to an action or force, greater than the force of gravity. (Internally or Externally produced) • The size, shape, and number of resulting stains will depend, primarily, on the amount of force utilized to strike the blood source. • This category can be further subdivided to include: – Arterial Gush or spurt – Cast-off stains – Impact spatter (medium or high velocity) Arterial gush or spurt • Bloodstain pattern (s) resulting from blood exiting the body under pressure from a breached artery. Cast-off Stains • Blood released or thrown from a blood-bearing object in motion (Knives, bludgeons) Projected blood through a syringe Impact Spatter • Blood stain patterns created when a blood source receives a blow or force resulting in the random dispersion of smaller drops of blood. • This category can be further subdivided into; – Low Velocity – Medium Velocity – High Velocity Low Velocity Impact Spatter •Gravitational pull up to 5 feet/sec. •Relatively large stains 4mm in size and greater Medium Velocity Impact Spatter • Force of 5 to 25 feet/sec. • Preponderant stain size 1 to 4mm in size High Velocity Impact Spatter Force of 100 feet/sec. and greater Preponderant stain size 1mm in size and smaller Mist like appearance 3. Transfer Bloodstains • A transfer bloodstain is created when a wet, bloody surface comes in contact with a secondary surface. • A recognizable image of all or a portion of the original surface may be observed in the pattern, as in the case of a bloody hand or footwear. THE END