H 2 - Digestion - IBDPBiology-Dnl
advertisement
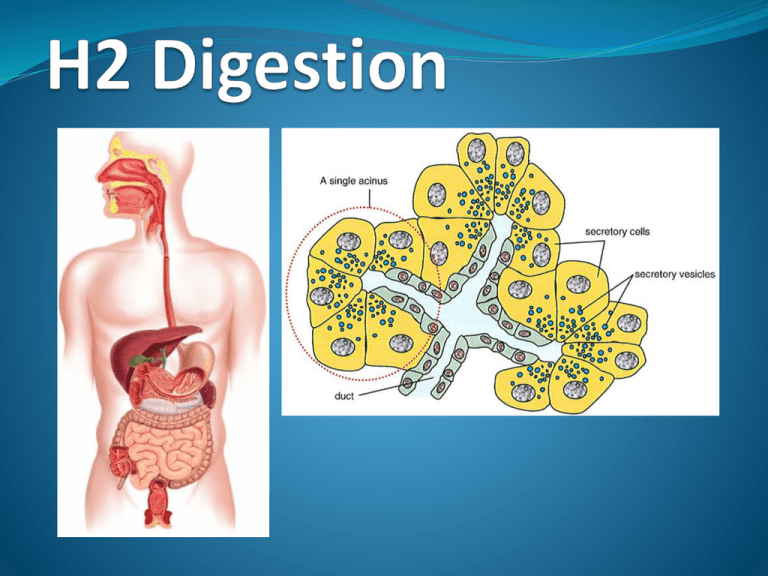
Assessment Statements H.2.1 State that digestive juices are secreted into the alimentary canal by glands, including salivary glands, gastric glands in the stomach wall, the pancreas and the wall of the small intestine. H.2.2 Explain the structural features of exocrine gland cells. H.2.3 Compare the composition of saliva, gastric juice and pancreatic juice. H.2.4 Outline the control of digestive juice secretion by nerves and hormones, using the example of secretion of gastric juice. H.2.5 Outline the role of membrane-bound enzymes on the surface of epithelial cells in the small intestine in digestion. H.2.6 Outline the reasons for cellulose not being digested in the alimentary canal. H.2.7 Explain why pepsin and trypsin are initially synthesized as inactive precursors and how they are subsequently activated. H.2.8 Discuss the roles of gastric acid and Helicobacter pylori in the development of stomach ulcers and stomach cancers. H.2.9 Explain the problem of lipid digestion in a hydrophilic medium and the role of bile in overcoming this. Secretion of digestive juices digestive juices are secreted into the alimentary canal by glands These glands includes; salivary glands,- secrets saliva gastric glands in the stomach wall,- secret gastric juice pancreas, - secrets pancreatic juice wall of the small intestine, secrets intestinal juice Structural features of exocrine gland cells Exocrine glands secrets into a space, lumen or duct The clustered secretary cells of an exocrine gland, arranged around the space into which secretion takes place, are called acini (sing. acinus) Secretory cells have a distinctive structure, the cyrtoplasm is packed with: rough endoplasmic reticulum (rER) which synthesis of proteins to be packaged for export many mitochondria – the source of the ATP necessary for the protein synthesis several Golgi apparatus – processing & packaging proteins from rER nucleoli in the nucleus – synthesis ribosomes for rER Group of acini with their ducts connecting together TEM of secretory cells of the exocrine glands of the pancreas By use of a table, compare the composition of saliva, gastric juice & pancreatic juice. Active ingredients, conditions required & outcome Secretion and gland Saliva salivary glands gastric juice gastric glands pancreatic juice pancreas Site of action mouth stomach pH 6.5 – 7.5 2.0 small 7.0 intestine enzymes & non-enzyme components substrate or effect product Amylase mucus Starch lubricates maltose Pepsin rennin (young mammals only) hydrochloric acid Proteins coagulates milk protein creates acidic environment that kills bacteria polypeptides Amylase proteases (trypsin & chymotrypsin) peptidases Starch proteins Maltose Polypeptides peptides & amino acids Lipases Triglycerides nucleases nucleotides polypeptides fatty acids & Glycerol pentose sugars, Pi & bases Control of gastric juice secretion by nerves & hormones. Control of gastric juice secretion by nerves & hormones chemoreceptors & stretch sight & smell of food initiate release of gastric juice before food is taken into the mouth i.e. before food reaches stomach, gastric juice is already secreted by reflex action receptors in gastric mucosa detect presence of food in the stomach impulses from these receptors are sent to brain, which sends impulses to gastric glands causing the release more gastric juice impulses are also sent to endocrine glands in gastric mucosa to release gastrin into the blood stream gastrin stimulates gastric glands to increase secretions of gastric juice gastric juices contains hydrochloric acid & pepsinogen low pH of stomach & hormones inhibits gastrin production through negative feedback mechanism The control of gastric secretion Role of membrane-bound enzymes some digestive enzymes such as maltase are immobilised in the plasma membrane of epithelial cells on the surface of intestinal villi enzyme immobilisation is when the enzyme molecule is attached to a fixed surface being fixed to the membrane of the gut epithelium is more efficient since the enzyme is not removed (reused) & can be linked to secondary functions such as membrane transport maltose binds into the active site of maltase on the cell membrane enzyme. maltose is hydrolysed into glucose molecules which are immediately absorbed into epithelial cells & pass into blood capillary Reasons for cellulose not being digested in the alimentary canal cellulose exists in plant cell walls it is insoluble in water, causing a problem with it’s digestion humans do not have enzyme cellulase thus they are not able to digest cellulose cellulose makes up the roughage or dietary fibre that is an essential component of our diet eventually, cellulose is egested along with other undigested materials as faeces Synthesis & activation of Pepsin & Trypsin pepsin and trypsin are protease enzymes if they were produced in an active form they would digest the exocrine cells that make them thus they are produced in an inactive form (precursors), pepsinogen & trypsinogen pepsinogen is activated by HCl while trypsinogen is activated by enterokinase Helicobacter pylori (H. pylori) Helicobacter pylori is a bacterium which enters the stomach & survives by attaching to receptors on the plasma membrane of the cells of the stomach mucosa, below the mucus lining in stomach, the bacteria are protected from strong acidity by: the mucus layer that lines the inner surface; secreting the enzyme urease which neutralized the acidic environment of the stomach by converting urea into the basic ammonia and buffer bicarbonate bacteria cells can't be destroyed by the body’s immune system because the mucus layer prevents antibodies from reaching the bacteria Roles of gastric acid & Helicobacter pylori in the development of stomach ulcers & stomach cancers. about 80 % of gastric ulcers are caused by Helicobacter pylori (H. pylori) H. pylori is a bacterium which causes gastritis i.e. inflammation of stomach lining stomach ulcers are open sores in the stomach wall lining prolonged presence of ulcers may lead to the formation of tumours cancer of the stomach is a malignant tumour in the stomach wall H. pylori survives in the stomach mucosa by producing urease which neutralizes gastric acid colonization by H. pylori opens up & weakens the protective mucus lining for digestive attack by gastric acid (HCl), causing ulcers linking H. pylori to stomach ulcers was a paradigm shift in medicine cause was previously thought to be stress, lifestyle, or diet H. pylori is now thought to be primary cause of gastric ulcers & is now treated as infectious disease Problem of lipid digestion in a hydrophilic medium & the role of bile in overcoming this lipids are strongly bile is a strongly alkaline hydrophobic & resist break-up into small droplets in a hydrophilic (aqueous) medium lipid molecules tend to coalesce forming droplets of fat lipase is water soluble but has an active site to which its hydrophobic substrate binds yellow green, mucous fluid containing the bile salts, bile pigments & cholesterol bile’s main role is to emulsify fats i.e. break fats into tiny droplets which enormously increases their surface area therefore increasing the rate at which it digest lipid bile also neutralises the acidity of the chyme Emulsification of fats bile salts are molecules with both hydrophilic & hydrophobic properties tiny spheres of lipid are formed, with the hydrophobic part of bile salts embedded in their surfaces, and the hydrophilic parts exposed to interact with water & prevent lipid molecules from coalescing with each other the droplets in this condition, known as micelles, remain suspended in an aqueous medium. this process is called emulsification Revision Questions Explain the structural Discuss the roles of gastric features of exocrine gland cells. [4] Compare gastric juice and pancreatic juice. [3] Outline the control of the secretion of gastric juice by nerves and hormones. [4] Outline the reason for one named substance found in food not being digested and absorbed by humans. [2] acid and Helicobacter pylori in the development of stomach ulcers and cancers. [5] Explain why trypsin is initially synthesized as an inactive precursor and how it is activated. [3] State two components of bile. [2] Explain the role of bile in lipid digestion. [2]