BME 412 Biomedical Signal Processing Class 1
advertisement
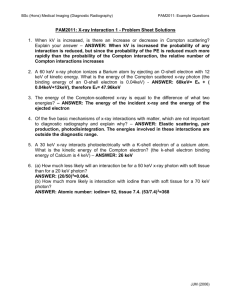
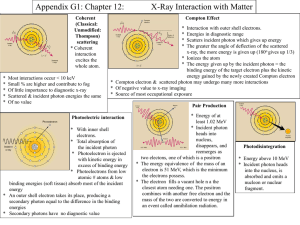
BME 560 Medical Imaging: X-ray, CT, and Nuclear Methods Radiation Physics Part 2 Today • EM Radiation interactions with matter – – – – Rayleigh scatter Photoelectric effect Compton scatter Pair production • Attenuation of EM Radiation X-ray interactions with matter Possible outcomes for an x-ray or gamma ray when traveling through matter are: – No effect (a) (it travels along the original path with original energy) (a) (b) (c) – Absorption (b) (it is absorbed in the matter) – Scatter (c) (It changes its direction of travel and/or energy) Imaging detector EM Radiation • Four possible interactions with matter – – – – Rayleigh scatter Photoelectric effect Compton scatter Pair production • Each has its own physical properties Rayleigh Scattering • Elastic (coherent, classical) scattering scatter with direction change but no energy loss. huincident = huscattered ; lincident = lscattered • Characteristics – an interaction of the x-ray with the entire atom via a refractory mechanism (wavelength ~ atomic radius) – occurs for longer wavelengths (low x-ray energies in the mammography range - 15 - 30keV) – reduces imaging quality in x-ray imaging. E(keV) P(%) ~30 <12 >70 <5 P: probability Compton scattering 1. It is also referred as inelastic or non-classical scattering 2. an interaction of incident x-ray with outer shell electrons; 3. almost atomic (proton) number (Z) independent; 4. proportional to re; 5. weakly energy dependent until energy is high (1MeV); 6. a disturbance to x-ray image quality. Compton Scatter Equation Planck’s constant l scattered l original h (1 cos ) m0c Scatter angle wavelengths Electron rest mass Compton Scattering energy and angular dependence Ee- hu0 f Energy and momentum conservation husc hu 0 hu 0 h u sc 1 hu 0 m 0c 2 E e hu 0 (1 cos ) 1 1 v /c m 0v c (1 cos ) hu 0 m0c 2 cos m0c 2 2 (1 cos ) 2 ( h u 0 h u sc cos ) f= 00 & = 1800 Compton scattering (Max energy transfer to electron) hu 0 2 E e (1 cos 180 ) 2 hu0 hu 0 f 2 m 0c m 0c hu 0 hu 0 hu 0 hu 0 1 (1 cos 180 ) 1 2 2 2 m 0c m 0c h u sc ,min h u 0 1 2 1 hu 0 m 0c ( h u 0 100 keV ; E e h u sc max 180 , h u 0 100 keV min 180, h u 0 100 keV husc ( h u 0 10 MeV ; 2 hu 0 m 0c 2 E e 0.2) 100 keV 2 0.2 1 2 0.2 h u sc Ee- max 180 , h u 0 10 MeV min 180, h u 0 100 keV 28 keV 100 keV 28 keV 72 keV hu 0 m 0c 2 20 ) 10 MeV 2 20 1 2 20 9.8 MeV 10 MeV 9.8 MeV 0.2 MeV = 900 Compton scattering hu 0 2 E e hu 0 (1 cos 90 ) 1 ( h u 0 10 MeV ; 1 hu 0 m 0c 2 hu 0 m 0c 2 E e 20 ) 90, h u 0 10 MeV min h u sc min 90, h u 0 10 MeV 90 1 20 90 , h u 0 100 keV 9.5 MeV 10 MeV 9.5 MeV 0.5 MeV 2 m 0 c 511 keV hu 0 m 0c 2 0.2) 100 keV h u sc 20 Ee- husc ( h u 0 100 keV ; 10 MeV h u sc f 2 m 0c m 0c hu 0 hu 0 hu 0 1 (1 cos 90 ) 1 2 2 m 0c m 0c h u sc ,min h u 0 E e hu0 hu 0 min 90, h u 0 100 keV 0.2 1 0.2 17 keV 100 keV 17 keV 83 keV Compton scatter angular distribution hu0 f Ee- husc The lower the incident x-ray energy, the more isotropic (angular distribution) the (compton) scattered x-ray is. (Isotropic - each point of compton interaction becomes an x-ray source - bad for imaging) Photoelectric Effect (PE) 1) An total absorption event (not a scatter): all or none; 2) An interaction of incident x-ray with inner shell electron; 3) Highly dependent on atomic (proton) number (Z) - Z3; 4) Highly energy dependent - E-3; Photoelectric effect • Incident electron deposits all of its energy into a shell electron – Must overcome electron binding energy • The shell electron (photoelectron) escapes – Ionization event – Energetic electron interacts with tissue (short range) • The photon must start with energy greater than the electron binding energy. Photoelectric Effect • “K-edges” – Photoelectric attenuation as a function of energy is discontinuous at the shell binding energies. – We make use of this property in several ways. From Sprawls, The Physical Basis of Medical Imaging Photoelectric effect energy and Z dependence High Z dependence (Z3) of PE is the basic reason why diagnostic x-ray is suited to medical imaging: – PE completely removes the incident x-ray (no scatter or partial absorption) – PE differentiates different atomic compositions in tissue (bone and fat); – PE is behind the use of high Z image contrast materials; – PE decreases drastically (E-3) with increasing x-ray energy (not good for imaging but good for therapy) X-ray imaging contrast ZBa=56; r =3.5g/cm3 Zwater, effective=7.25; r =1g/cm3 (ZBa/Zwater)3=512 Pair Production • occurs under strong electric field of nucleus (=>Z dependent); • only occurs if the incident x-ray energy is > 1.022MeV (enough to create the rest masses of an e- and a e+); • completely removes the incident x-ray (no scatter or partial absorption) • increases with increasing x-ray energy • generates an electron and a positron Positron annihilation 2nd part of fig 3-12, redbook • Positron annihilation gamma rays are ~1800 apart; • each gamma ray has 511keV; • principle of PET scanner (a measure of PET agent distribution in patient). EM Radiation Interactions • Rayleigh scatter: only significant at low energies • Compton scatter: dominates at imaging energies • Photoelectric effect: significant at imaging energies • Pair production: cannot occur at imaging energies Total linear attenuation coefficient N x N 0e x Rayleigh photoelectric compton pair Soft Tissue productin X-ray attenuation n N Dx D N N Absorbed & scattered n transmitted N-n Dx Dx N ln N x N x N 0e N t N 0e ( l : decay l t cons tan t ) x Linear attenuation coefficient (cm-1): 0.10cm-1 ==> 10% per cm. Total attenuation coefficients of water and lead Characteristic x-ray peak (K-shell) Table of interaction vs. x-ray energy (Khan?) Relative importance of each x-ray interaction in water Mass attenuation coefficient (/r) linear attenuation coefficient () normalized to the density (r) of the irradiated material. Therefore it is independent of density. /r (cm2/g) = (cm-1) /r (g/cm3) Nx = N0 e- (/r)rx Exercise Given: CT x-ray energy is120kVp. The patient thickness is 20 cm and 25 cm in the AP and lateral direction, respectively. If the x-rays attenuate 20% per cm of tissue, what is the xray intensity difference as measured by the detector in the AP and lateral positions? xap patient xat Solution: 0.20 cm-1 N x N 0e N ap X-ray detector N lateral e 0.2 5 x e 20 e 25 e e 2.72 ( 25 20 ) Half Value Layer (HVL) N HVL N 0 / 2 N 0 e HVL (T1 / 2 ln 2 ln 2 l ( / r ) r HVL 0.693 100 (a)(b) (c) ) HVL • HVL or is a function of BOTH the x-ray (E) and the matter (Z,r). • T1/2 is a function of radionucleus only. 50 = 100/2 Narrow-beam and broad-beam HVL • which HVL is larger, broad-beam or narrow-beam? Polyenergetic x-ray beam Beam Hardening: HVL (x) • Beam hardening - mean energy of a poly energetic x-ray beam increases as it travels through the irradiated material. • Reason - lower energy x-rays have larger than higher energy x-rays and thus attenuate quicker. • HVL(x1) < HVL (x2) when x1 < x2 (for polyenergetic x-ray beams) Review of interactions Particles (electrons) • Collisional – Ionization, heat • Radiative – X-rays (characteristic, Bremsstrahlung) EM • Rayleigh scatter – Change direction, no energy loss • Compton scatter – Change direction, energy loss • Photoelectric – Absorption, photoelectron released • Pair production – Absorption, electron-positron pair released