Radiation Interactions
advertisement

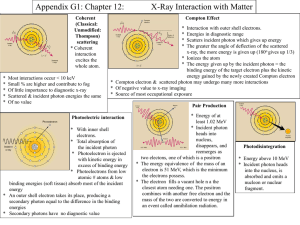
Radiation Interactions Robert Metzger, Ph.D. Interactions with Matter Charged particles lose energy as they interact with the orbital electrons in matter by excitation and ionization, and/or radiative losses. Excitation occurs when& the incident particle bumps an electron to a higher orbital in the absorbing medium. Ionization occurs when the transferred energy exceeds the binding energy of the electron and it is ejected. The ejected electron may then also produce further ionizations. Specific Ionization The number of ion pairs produced per unit path length is the specific ionization. Alpha particles can produce as many as 7,000 IP/mm. Electrons produce 50-100 IP/cm in air. LET is the product of the specific ionization and the average energy deposited per IP [IP/cm x eV/IP]. About 70% of electron energy loss leads to non-ionizing excitation. Charged Particle Tracks e- follow tortuous paths through matter as the result of multiple Coulombic scattering processes An α2+, due to it’s higher mass follows a more linear trajectory Path length = actual distance the particle travels in matter Range = effective linear penetration depth of the particle in matter Range ≤ path length c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2 nd ed., p.34. Bremsstrahlung Deceleration of an e- around a nucleus causes it to emit Electromagnetic radiation or bremsstrahlung (G.): ‘breaking radiation’ Probability of bremsstrahlung emission Z2 Ratio of e- energy loss due to bremsstrahlung vs. excitation and ionization = KE[MeV]∙Z/820 Thus, for an 100 keV e- and tungsten (Z=74) ≈ 1% c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2 nd ed., p.35. Electromagnetic Radiation Interactions Raleigh Scattering: Photon is scattered with no energy loss. Uncommon at diagnostic energies. Compton Scattering:Photon strikes outer electron and ejects it, resulting in energy loss of photon and change of direction. Photoelectric Effect: Photon is totally absorbed by K or L shell electron which is ejected. Pair Production: High energy photon interaction. Rayleigh Scattering Excitation of the total complement of atomic electrons occurs as a result of interaction with the incident photon No ionization takes place No loss of E <5% of interactions at diagnostic energies. c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2 nd ed., p. 37. Compton Scattering Dominant interaction of x-rays with soft tissue in the diagnostic range and beyond (approx. 30 keV 30MeV) Occurs between the photon and a “free” e- (outer shell e- considered free when Eg >> binding energy, Eb of the e- ) Encounter results in ionization of the atom and probabilistic distribution of the incident photon E to that of the scattered photon and the ejected e A probabilistic distribution determines the angle of deflection c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2 nd ed., p. 38. Compton Scattering Compton interaction probability is dependent on the total no. of e- in the absorber vol. (e-/cm3 = e-/gm · density) With the exception of 1H, e-/gm is fairly constant for organic materials (Z/A 0.5), thus the probability of Compton interaction proportional to material density () Conservation of energy and momentum yield the following equations: Eo = Esc + Ee- Esc = E0 E0 1+ 1- cosθ 2 m ec , where mec2 = 511 keV Compton Scattering As incident E0 both photon and e- scattered in more forward direction At a given fraction of E transferred to the scattered photon decreases with E0 For high energy photons most of the energy is transferred to the electron At diagnostic energies most energy to the scattered photon Max E to e- at of 180o; max E scattered photon is 511 keV at of 90o c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2nd ed., p. 39. Photoelectric Effect All E transferred to e- (ejected photoelectron) as kinetic energy (Ee) less the binding energy: Ee = E0 – Eb Empty shell immediately filled with e- from outer orbitals resulting in the emission of characteristic x-rays (Eg = differences in Eb of orbitals), for example, Iodine: EK = 34 keV, EL = 5 keV, EM = 0.6 keV c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2nd ed., p. 41. Photoelectric Effect Eb Z2 Photoe and cation; characteristic x-rays and/or Auger e Probability of photoe- absorption Z3/E3 (Z = atomic no.) Explains why contrast as higher energy x-rays are used in the imaging process Due to the absorption of the incident x-ray without scatter, maximum subject contrast arises with a photoe- effect interaction Increased probability of photoe- absorption just above the Eb of the inner shells cause discontinuities in the attenuation profiles (e.g., K-edge) Photoelectric Effect c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 1 st ed., p. 26. Photoelectric Effect Edges become significant factors for higher Z materials as the Eb are in the diagnostic energy range: Contrast agents – barium (Ba, Z=56) and iodine (I, Z=53) Rare earth materials used for intensifying screens – lanthanum (La, Z=57) and gadolinium (Gd, Z=64) Computed radiography (CR) and digital radiography (DR) acquisition – europium (Eu, Z=63) and cesium (Cs, Z=55) Increased absorption probabilities improve subject contrast and quantum detective efficiency At photon E << 50 keV, the photoelectric effect plays an important role in imaging soft tissue, amplifying small differences in tissues of slightly different Z, thus improving subject contrast (e.g., in mammography) Pair Production Conversion of mass to E occurs upon the interaction of a high E photon (> 1.02 MeV; rest mass of e- = 511 keV) in the vicinity of a heavy nucleus Creates a negatron (β-) - positron (β+) pair The β+ annihilates with an e- to create two 511 keV photons separated at an of 180o c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2nd ed., p. 44. Radiation Interactions A B WHICH IS HIGH kVp CHEST RADIOGRAPH AND WHICH IS LOW kVp CHEST RADIOGRAPH ? Compton vs Photoelectric A B WHICH IS LOW kVp BONE RADIOGRAPH AND WHICH IS HIGH kVp BONE RADIOGRAPH ? Linear Attenuation Coef Cross section is a measure of the probability (‘apparent area’) of interaction: (E) measured in barns (10-24 cm2) Interaction probability can also be expressed in terms of the thickness of the material – linear attenuation coefficient: (E) [cm-1] = Z [e- /atom] · Navg [atoms/mole] · 1/A [moles/gm] · [gm/cm3] · (E) [cm2/e-] (E) as E , e.g., for soft tissue (30 keV) = 0.35 cm-1 and (100 keV) = 0.16 cm-1 (E) = fractional number of photons removed (attenuated) from the beam by absorption or scattering Multiply by 100% to get % removed from the beam/cm Attenuation Coefficient An exponential relationship between the incident radiation intensity (I0) and the transmitted intensity (I) with respect to thickness: I(E) = I0(E) e-(E)·x total(E) = PE(E) + CS(E) + RS(E) + PP(E) At low x-ray E: PE(E) dominates and (E) Z3/E3 At high x-ray E: CS(E) dominates and (E) Only at very-high E (> 1MeV) does PP(E) contribute The value of (E) is dependent on the phase state: water vapor << ice < water Attenuation Coefficient c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2 nd ed., p. 46. Mass Attenuation Coef Mass attenuation coefficient m(E) [cm2/g] – normalization for : m(E) = (E)/Independent of phase state () and represents the fractional number of photons attenuated per gram of material - (E)··x I(E) = I0(E) e m Represent “thickness” as g/cm2 - the effective thickness of 1 cm2 of material weighing a specified amount (·x) Half Value Layer Thickness of material required to reduce the intensity of the incident beam by ½ ½ = e-(E)·HVL or HVL = 0.693/(E) Units of HVL expressed in mm Al for a Dx x-ray beam For a monoenergetic incident photon beam (i.e., that from a synchrotron), the HVL is easily calculated Remember for any function where dN/dx N which upon integrating provides an exponential function (e.g., I(E) = I0(E) ∙ e±k·w ), the doubling (or halving) dimension w is given by 69.3%/k% (e.g., 3.5% CD doubles in 20 yr) For each HVL, I by ½: 5 HVL I/I0 = 100%/32 = 3.1% Mean Free Path Mean free path (avg. path length of x-ray) = 1/ = HVL/0.693 Beam hardening The Bremsstrahlung process produces a wide spectrum of energies, resulting in a polyenergetic (polychromatic) x-ray beam As lower E photons have a greater attenuation coefficient, they are preferentially removed from the beam Thus the mean energy of the resulting beam is shifted to higher E c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 1st ed., p. 281. Effective Energy The effective (avg.) E of an x-ray beam is ⅓ to ½ the peak value (kVp) and gives rise to an eff, the (E) that would be measured if the x-ray beam were monoenergetic at the effective E Homogeneity coefficient = 1st HVL/2nd HVL A summary description of the x-ray beam polychromaticity HVL1 < HVL2 < … HVLn; so the homogeneity coefficient < 1 c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2nd ed., p. 45. c.f. Bushberg, et al. The Essential Physics of Medical Imaging, 2nd ed., p. 43. Shielding I = BI0 e-x I is the Intensity in shielded area I0 is the unattenuated intensity B is the buildup factor is the attenuation coefficient X is the shield thickness Shielding The buildup factor is the ratio of scattered photons that scatter back into the beam. Since the photoelectric effect dominates at diagnostic x-ray energies, the buildup factor is 1.0. Therefore lead aprons work well in diagnostic x-ray, but not in Nuclear Medicine (140 keV gammas) Buildup must be considered for PET.