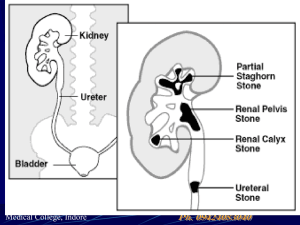
Urolithiasis
or
Urinary Calculi
Refers to the presence of
stones in the urinary
system
Stones, or calculi, are
formed in the urinary
tract from the kidney to
bladder by the
crystallization of
substances excreted in
the urine.
Pathophysiology and Etiology
1. Most stones (75%) are composed mainly
of calcium oxalate crystals;
the rest are composed of calcium
phosphate salts, uric acid, struvite
(magnesium, ammonium, and phosphate)
2. Causes and predisposing factors.
Hypocalcemia and hypercalciuria caused
by hyperparathyroidism, renal tubular
acidosis, multiple myeloma, and excessive
intake of vitamin D, milk and alkali.
Chronic dehydration, Poor fluid intake, and
immobility.
Diet high in purines and abnormal purine
metabolism. (Hyperuricemia and gout)
Genetic predisposition for urolithiasis /
genetic disorders. (Cystinuria)
Chronic infection with urea – splitting
bacteria (Proteus vulgaris)
Chronic obstruction with stasis of urine,
foreign bodies within the urinary tract.
Excessive oxalate absorption in
inflammatory bowel disease and bowel
resection or ileostomy.
Living in mountainous, desert, or tropical
areas.
3. Stones may be found anywhere in the
urinary system and vary in size from mere
granular deposits (called sand or gravel) to
bladder stones the size of an orange.
4. Three out of four patients with stones are
men; in both sexes, the peak age of onset
is between ages 20 and 40.
5. Most stones migrate downward (causing
severe colicky pain) and are discovered in
the lower ureter. Spontaneous stone
passage can be anticipated in 80% of pts
with urolithiasis.
6. Some stones may lodge in the renal
pelvis, ureters, or bladder neck causing
obstruction, edema, secondary infection
and, in some cases, nephron damage.
7. People who have had two stones tend to
have recurrences.
Clinical Manifestations
Pain pattern depends on site of
obstruction.
a. Renal stones produce an increase in
hydrostatic pressure and distention of the
renal pelvis and proximal ureter causing
renal colic. Pain relief is immediate after
stone passage.
b. Large ureteral stones produce
symptoms or obstruction as they pass
down the ureter (ureteral colic)
c. Bladder stones produce symptoms similar
to cystitis.
Obstruction – stones blocking the flow of
urine will produce symptoms of UTI; chills
and fever.
GI symptoms include nausea, vomiting,
diarrhea, abdominal discomfort – due to
renointestinal reflexes and shared nerve
supply (celiac ganglion) between the
ureters and intestine.
Assessment Factors Specific to
Patients with Urinary calculus
Diseases
Present & Past
medical history
Medical treatment &
surgical procedures
on and outside GU
tract.
UTIs
Periods of prolonged
illness with
mobilization /
dehydration
Gout
Malignant neoplasms
Endocrinopathies
Family histories
Present & Past
geographic residences
Age
Sex
Occupation
Dietary habits
Fluid Intake
Vitamin Intake
Medication History
Steroids
Alkalizing agents
Pain
Location
Intensity
Character & Quality
Chronology
Pain response
Psychological
Behavioral
Affective
Surgical Intervention for
Urolithiasis
Surgery
Open Procedures
Nephrolithotomy
Nephrectomy (partial /
total)
Pyelolithotomy
Ureterolithotomy
Custolithectomy
Litholapaxy
Indications
Crushing of urolithiasis
with lithotrite; small stone
fragment can then be
flushed from UT
Closed procedures
Percutaneous
Ultrasonic lithotripsy
(PUL)
Extracorporeal shock
wave lithotripsy
(ESWL)
Ultrasound used to
fragment large calculus
so fragments can be
mechanically removed
or flushed out of the
system.
Patient is placed in tank
of water through which
shock waves are sent
to pulverize stone that
is then passed during
urination.
Nursing Diagnoses
Acute pain related to inflammation,
obstruction, and abrasions of UT by
migration of stones.
Impaired Urinary Elimination related to
blockage of urine flow by stones.
Risk for Infection related to obstruction of
urine flow and instrumentation during
treatment.
Nursing Interventions
Controlling Pain
1. Give opioid analgesic (usually IV or IM)
until cause of pain can be removed.
a. Monitor pt closely for increasing pain;
may indicate inadequate analgesia.
b. Very large doses of opioids are typically
required to relieve pain, so monitor for
respiratory depression and drop in blood
pressure.
2. Encourage pt to assume position that
brings some relief.
3. Reassess pain frequently.
4. Administer antiemetics (IM or rectal
suppository) as indicated for nausea.
Maintaining Urine Flow
1. Administer fluids orally or IV (if vomiting)
to reduce concentration of urinary
crystalloids and ensure adequate urine
output.
2. Monitor total urine output and patterns of
voiding. Report oliguria or anuria.
3. Strain all urine through strainer or gauze
to harvest the stone. Uric acid stones
may crumble. Crush clots, and inspect
sides of urinal / bedpan for clinging
stones / fragments.
Patient Education and Health
Maintenance
Recovery from surgical Interventions for
Stone Disease
1. Encourage fluids to accelerate passing of
stone particles.
2. Teach about analgesics that still may be
necessary for colicky pain, which may
accompany passage of stone debris.
3. Warn that some blood may appear in
urine for several weeks.
4. Encourage frequent walking to assist in
passage of stone fragments.
5. Teach pt to strain urine through a coffee
filter.
6. For outpatient treatment, the patient may
use a coffee filter to strain urine.
7. Help pt to walk, if possible, because
ambulation may help move the stone
through the UT.
Avoid over hydration, which may result in
increased distension at stone location,
causing an increase in pain and
associated symptoms.
Prevention of Recurrent Stone
Formation
1. For pts with calcium oxalate stones
a. Instruct on diet – avoid excess of calcium and
phosphorus; maintain a low sodium diet (sodium
restriction decreases amount of calcium absorbed
in intestine)
b. Teach purpose of drug therapy – thiazide diuretics
to reduce urine calcium excretion, allopurinol
therapy to reduce uric acid concentration.
2. For pts with uric acid stones
a. Teach methods to alkalinize urine to
enhance urate solubility.
b. Instruct on testing urine pH.
c. Teach purpose of taking allopurinol – to
lower uric acid concentration.
d. Provide information about reduction of
dietary purine intake (low protein – red
meat, fish, fowl)
3. For pts with infection (Struvite) stone
a. Teach signs and symptoms of urinary
infection; encourage him to report infection
immediately; must be treated vigorously.
b. Try to avoid prolonged periods of
recumbency – slows renal drainage and
alters calcium metabolism.
c. Teach pt with drug therapy with D –
Pencillamine (Depen) – to lower cystine
concentration, or dissolution by direct
irrigation with thiol derivatives.
d. Explain importance of maintaining drug
therapy consistently.
4. For all pts with stone disease,
a. Explain need for consistently increased
fluid intake (24 – hour urinary output
greater than 2l) – lowers the
concentration of substances involved in
stone formation.
i.
Drink enough fluids to achieve a urinary
volume of 2000 – 3000 ml or more every 24
hours.
ii.
Drink larger amounts during periods of
strenuous exercise, if pt perspires freely.
iii. Take fluids in evening to guarantee a high
urine flow during the night.
b. Encourage a diet low in sugar and animal
proteins – refined carbohydrates appear to
lead to hypercalciuria and urolithiasis;
animal proteins increase urine excretion of
calcium, uric acid, and oxalate.
c. Increase consumption of fiber – inhibits
calcium and oxalate absorption.
d. Save any stone passed for analysis. (Only
pts with more than one episode of
urolithiasis are advised to have a
metabolic evaluation.)
e. Can discontinue urine straining 72 hours
after symptoms resolve.
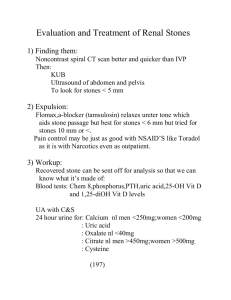
Management
1. If small stone (< 4 mm) and able to
treat as out pt, 80% will pass stone
spontaneously with hydration,
pain control, and reassurance.
2. Hospitalized for intractable pain,
persistent vomiting, high – grade
fever, obstruction with infection,
and solitary kidney with infection.