Pediatric renal stones --- 23/11/2014
advertisement

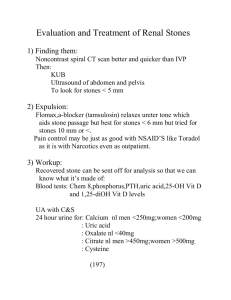
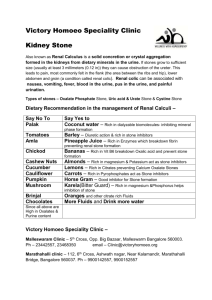
Pediatric renal stones Safaa. M Abdel Rahman MD Lecturer of pediatric nephrology Cairo university Pediatric renal stones Definitions Epidemiology Types Aetiology Genetic basis Clinical presentations Diagnosis Management Definitions Urolithiasis, kidney stones, renal stones, and renal calculi are interchangeably used to refer to the accretion of hard, solid, nonmetallic minerals in the urinary tract Nephrocalcinosis is a term that refers to increased calcium content in the parenchyma of the kidney Epidemiology Children can present with stones at any age (eg, premature newborn to teenager). In children, calcium stones are most common. The approximate frequency of kidney stone types in the pediatric age group is calcium with phosphate or oxalate (57%), struvite (24%), uric acid (8%), cystine (6%), endemic (2%), mixed (2%), and other types (1%). With children, particularly younger children, the primary cause of stone formation (eg, hypercalciuria, hyperuricosuria) can usually be identified with a through evaluation. Type Calcium with phosphate or oxalate Purine derivatives Magnesium ammonium phosphate (struvite) Cysteine Combinations of the preceding items Drugs or their metabolites (eg, phenytoin, triamterene) Melamine-contaminated milk powder consumption Aetiology Renal stones occur as a result of the following 3 factors: Supersaturation of stone-forming compounds in urine Presence of chemical or physical stimuli in urine that promote stone formation Inadequate amount of compounds in urine that inhibit stone formation (eg, magnesium, citrate) Aetiology Risk factors Habitually low urine volume High urine excretion of calcium High urine excretion of uric acid High urine excretion of oxalate Low urine pH: Uric acid and cysteine are less soluble in acid urine. High urine pH: Struvite and calcium phosphate are less soluble in alkaline urine. Drugs and stone formation Mechanism of Stone Formation Drug Primary Stone Composition Crystallization of highly excreted, poorly soluble drug or metabolite causes stone formation. Phenytoin, triamterene, sulfonamides, felbamate, ceftriaxone, indinavir, ciprofloxacin, guaifenesin/ephedrine Drug or its metabolites Drug may increase the concentration of stone-forming minerals. 1. Anti-cancer drugs 1. Uric acid 2. Glucocorticoid 2. Calcium 3. Allopurinol (if used in tumor lysis) 3. Xanthine 4. Loop diuretics 4. Calcium oxalate 5. Calcium and vitamin D 5. Calcium Drug inhibits activity of carbonic Topiramate, zonisamide, acetazolamide anhydrase enzymes in the kidney, causing metabolic acidosis, hypocitraturia, and elevated urine pH. Calcium phosphate Clinical presentation The size of the stone (larger stones tend to be more symptomatic, although some large stones produce few symptoms) The location of the stone The production of urinary outflow obstruction The movement of the stone (eg, from the renal pelvis to bladder) The presence of infection Clinical presentation The following are 5 fairly typical presentations of stone disease in children: 1. Intense pain that suddenly occurs in the back and radiates downward and centrally toward the lower abdomen or groin 2. Hematuria, usually gross, occurring with or without pain: Hematuria may or may not be present. 3. Infection leading to radiologic imaging in which a stone is identified Clinical presentation 4. Asymptomatic stones, which are sometimes identified when abdominal imaging is performed for another reason 5. Persistent microscopic hematuria, which consists of 5 or more RBCs per high-power field in 3 of 3 consecutive centrifuged urine specimens obtained at least 1 week apart Diagnosis History Frequent urinary tract infections frequent bouts of abdominal pain, hematuria (gross or microscopic), passage of previous calculus dietary intake (eg, oxalate, purine, calcium, phosphate, fructose, animal protein) drug intake (eg, anticancer drugs, glucocorticoids, allopurinol, loop diuretics), vitamin intake (A, D), fluid intake habitual fluid type (eg, water, milk, tea, sports drinks), The history should also include questions on chronic disease (eg, renal tubular acidosis, inflammatory bowel disease, short-gut syndrome, intractable seizures, cystic fibrosis), prior urologic surgery (eg, kidney transplant), or recent immobilization. Diagnosis Examinations Wt Ht Examination for 2ry cause - Distal renal tubular acidosis -Oxalosis -IBD -Cystic fibrosis -Short-gut syndrome Diagnosis laboratory studies: Complete blood count (CBC) Electrolyte, blood urea nitrogen (BUN), creatinine, calcium, phosphorus, alkaline phosphatase, uric acid, total protein, albumin, parathyroid hormone (PTH), and vitamin D metabolite levels Diagnosis laboratory studies: Spot urine analysis and culture, including ratio of calcium, uric acid, oxalate, cystine, citrate, and magnesium to creatinine Urine tests, including a 24-hour urine collection for calcium, phosphorus, magnesium, oxalate, uric acid citrate, cystine, protein, and creatinine clearance Uric acid /Glomerular >yrs <0.5mguric acid /dl of glomerular filtrate Calculated as uric acid x serum creatinine urine creatinine Diagnosis Imaging Renal ultrasonography is very effective for identifying stones in the urinary tract. Generally, ultrasonography should be used as a first study. If no stone is found but symptoms persist, helical (spiral) computed tomography (CT) scanning is indicated. Noncontrast spiral CT scanning is the most sensitive test for identifying stones in the urinary system. It is safe, rapid, and has been shown to have 97% sensitivity and 96% specificity. Plain abdominal x.ray . Intravenous pyelography is rarely used in children. Diagnosis Diagnosis Evaluation of Stones Attempting to obtain a stone for histologic and crystallographic evaluation is essential B.Hoppe, and Milliner , 2009 Treatment Managements Aim 1. To prevent additional renal damage, which may lead to loss of renal parenchyma 2. To manage pain associated current stone(s) 3. To expedite passage or removal of any stones present 4. To prevent new stones from forming. Managements A. Conservative therapy B. Surgical management of urolithiasis C. Medical treatment D. Monitoring Managements A. Conservative therapy Obstructed renal stone Non obstructed renal stone Managements A. Conservative therapy High fluid intake Diet A restriction of minerals after stone analysis Calcium stone: sodium and animal protein restriction Excessive intake D is to be avoided hyperuricosuria may benefit from avoiding purine-rich foods Managements B. Surgical management of urolithiasis The specific aims of surgical care drainage of the urinary tract removal of stones present in the urinary tract surgical correction of anatomic abnormalities Managements C. Medical 1. 2. Idiopathic hypercalciuria Renal tubular calcium leak thiazid therapy gastrointestinal (GI) absorptive and a low-calcium diet does not return urinary calcium levels to the reference range, neutral sodium phosphate Hypocitraturia oral potassium citrate. Managements Medical Struvite stones appropriate antibiotic. Surgical intervention or ESWL may be necessary Uric acid stone 1. Alkalinization of urine with sodium bicarbonate or potassium citrate in 4 divided doses (5-15 mL diluted in up C. to 6 oz water/juice PO PC & HS PRN 2. Xanthine oxidase inhibitors (Allopurinol) 10 mg/kg/day PO divided q12hr Managements Monitoring Effects of treatment should be monitored by measurement of urinary and plasma chemistries 1 month after initiating treatment and then every 2 months until a steady state is established. Children on calcium restriction should have serum calcium, parathyroid hormone (PTH), and urine calcium excretion determined at onset, in 2 months, and then at 6-month intervals. Managements Monitoring Children receiving thiazides should have serum electrolytes, cholesterol, uric acid, and urinary calcium excretion measured at onset, at 2 months, and then at 6month intervals. Children receiving allopurinol should have a complete blood count (CBC), liver function tests, and urinary uric acid excretion tests performed every 2 months. Managements Monitoring Patients should undergo annual imaging with renal ultrasonography to look for new or growing stones. Because of increased incidence of low bone density in children with hypercalciuria and nephrolithiasis, (DEXA) scanning should be performed at onset and then yearly in children aged 5 years and older. (Schwaderer et al 2008)