Haematuria
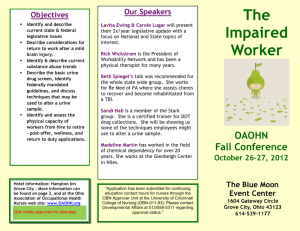
advertisement

Haematuria Miguel Cabalag Red Urine ©2011 UpToDate® Definition • Macroscopic (gross) – Red – brown urine • Microscopic – ≥3 RBC per high-power field on microscopic evalation of urinary sediment. Glomerular vs Extra-glomerular Glomerular Extra-Glomerular Colour Red/smoky brown/Coke Red/Pink Clots Absent May be present Proteinuria <500 mg/d May be >500 mg/d RBC casts Present Absent RBC morphology Dysmorphic Normal Adapted from ©2011 UpToDate® Anatomy DDx ©2010 UpToDate® DDx (Macroscopic) • MINTSIC – – – – – – – Medical (GN, AF) Infection (acute – UTI; chronic – TB, schistosomiasis) Neoplasm (benign, malignant, PCKD) Trauma Stones Iatrogenic (previous urological surgery) Coagulopathy • Excessive exercise • Transient unexplained DDx (Microscopic) • Glomerulonephritis – IgA Nephropathy – Post-streptococcal GN – Thin Basement membrane Disease – Membrano-proliferative GN Hx • Characteristics: – Colour, ?clots, timing (intermittent/terminal/start/independent), duration, etc • Infection: f/c/r, Irritative sx - frequency, urgency, nocturia, dysuria, incontinence (urge), flank/suprapubic/penile pain, sexual hx, urethral dc • Stones: renal colic • Prostate: Obstructive Sx • Malignancy: ?Painless, LOW, LOA, night sweats, smoking/ETOH/exposure to industrial dyes/cyclophosphamide (Bladder Ca) • Hx of trauma • Coagulopathy: easy bruising, bleeding elsewhere, FHx, prev dental procedures Hx ctd • GN: Recent URTI/sore throat (post infx GN/IgA nephropathy), haemoptysis/SOBOE (Goodpasture’s, Wegener’s granulomatosis), frothy urine (proteinuria), SOA • Medications (warfarin, cyclophosphamide, rifampicin, chemoTx) • Recent urological surgery • PHx: T2DM, AF, Sickle Cell anaemia • FHx of renal disease (PCKD) • Exclude other sources: ?period, ?malaena/haematochezia O/E • General: well/unwell, restless (colic), anaemia • Obs: haemodynamically stable, ?febrile • Abdo: peritonism, organomegaly, pain on ballotment of kidneys, flank pain, LA • Genito-urinary: ?urethral discharge, period • DRE: prostate, (? GIT source) • Resp: consolidation (?pneumonia) • CVS: AF, stigmata of Infx Endocarditis • Urinalysis: blood, leuc, nitrites, protein, glucose Ix • Bloods: – FBE + film, UEC, CMP, Uric Acid, PSA, LFTs (ALP), Glucose, CRP, ESR, Coags • Urine: – MCS (glom vs non-glom), Cytology, PCR (gonorrhoea/chlamydia) • Imaging: – – – – CT-KUB (non contrast – stones) CT-IVP (filling defect – malignancy) Renal tract USS XR-KUB • Cystoscopy Case 1 • 65 yo male p/w 3/52 history of red coloured urine. Intermittent, painless, present throughout stream. No obstructive/irritative sx. Otherwise well. • PHx: Nil significant • Meds: Glucosamine, Cholecalciferol • Smoker (50 pk yrs) • ETOH (2 stubbies/d) – DDx? DDx • MALIGNANCY! – Renal Cell Ca – Bladder TCC • GN Ix? Ix • Bloods: FBE, UEC, CMP, LFT (ALP) • Urine: MCS, Cytology • Imaging: – Flex Cystoscopy – CT-IVP • Staging (TNM) – Lung, liver, bone – CT-Abdo/Pelvis – CXR – Bone scan Staging Rx • Stage 1 (Ta/T1): TURBT +/- intravesical therapy (BCG) • Stage 2 (>T2) (muscle invasive disease): Neoadjuvant chemotherapy + Radical cystectomy with urinary diversion (ileal conduit) – Bladder sparing: Complete TURBT + RT + Chemo • Chemotherapy: – Methotrexate, vinblastine, doxorubicin, cisplatin (MVAC) – Gemcitabine + cisplatin (GC) • TCC: Long term surveillance (Field effect) Take home message • Painless haematuria in >40 yo = malignancy until proven otherwise Case 2 • 30 yo male, p/w red coloured urine a/w abdominal pain. • Further hx? Case 2 • HOPC: Severe 10/10 L flank pain radiating down to groin, intermittent. Truck driver (high protein, low fluid intake) • PHx: HTN, Obesity, Gout, T2DM • Meds: Thiazide, Allopurinol, Metformin, Aspirin • Smoker (40 pk yrs) • ETOH (4 glasses of red wine/d) • FHx of nephrolithiasis Common sites: (PUJ, VUJ, pelvic brim) Case 2 • Ix: – Bloods: FBE, UEC, CRP, CMP, Uric Acid – Urine: FWT, MCS – Imaging: • Non-contrast CT-KUB Mx • • • • • • • • • When to refer to Urology: – >5 mm/Staghorn/stone doesn’t pass/infection + obstruction/urosepsis/ARF/Solitary kidney/Bilateral obstruction Analgesia – Paracetamol, NSAIDs (Indomethacin Suppository), Opioids (oral/SC/IV) Anti-emetics IVF Medical therapy: CCB (Nifedipine), alpha blockers (Tamsulosin) Surgical: – Extracorporeal Shock Wave Lithotripsy (ESWL)*/Ureterscopic lithotripsy/Percutaneous nephrolithotomy Send stone for analysis Dietary modifications (inc fluid intake) Urine modification: – Ca stones: Thiazide diuretic and low Na diet – Uric Acid stones: Allopurinol – Cystine stones: Alkalinization of urine (Ural – NaHCO3/Potassium Citrate) Mx • Stone radiopauqe? – No Probable uric acid stone • Fluids + Analgesia; Alkalinize urine w Potassium Citrate – Yes Fluids + Analgesia stone >5mm? • Yes Refer to Urology – Staghorn Calculus Percutaneous lithotomy + ESWL – Calyceal/Upper ureteral calculus ESWL – Distal ureteral calculus Ureteroscopy/ESWL • No Strain urine and continue hydration + analgesia. Await stone to pass – Renal Tract USS in 2/52 if hydronephrosis/multiple stones on initial evaulation Nephrolithiasis • Composition: – 80%: Ca stones: • Ca oxalate • CaPO4 – Uric Acid (RADIOLUCENT) – Struvite (Mg, Ammonium, PO4) – Cystine Questions?