1- Systemic antifungals
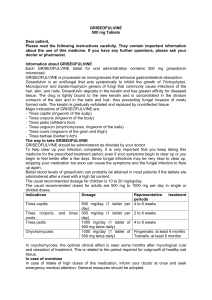
advertisement

ANTIFUNGALS IHAB YOUNIS,M.D. Classification 1- Systemic antifungals 2-Topical antifungals 1- Systemic antifungals Oral antifungal medications may be required for a fungal infection if : • It is extensive or severe • It resists topical antifungal therapy • It affects hair-bearing areas (tinea capitis and tinea barbae) Medications only suitable for dermatophyte infections • Griseofulvin • Terbinafine Griseofulvin )Ultragriseofulvin® , Fulvin ® 125 mg) • It has been available since 1958 • It comes from the mould, Penicillium griseofulvum • It is fungistatic i.e. stops fungal cells dividing but does not kill them outright. This means treatment needs to be continued for several weeks or months • It is not very well absorbed from the gut so, should be taken after a meal or milk as fat increases the absorption • The medication is carried into the skin by sweat and within a couple of weeks is concentrated in the outer skin layers • Half the medication is cleared from the blood stream in 10 to 20 hours. This means that: – the medication can be taken once daily – Griseofulvin should be continued until the fungal infection has completely gone because the medication is quickly cleared from skin and hair when it is stopped Dose regimen • Adults: 330-375 mg daily • Children: 10: 25 ultramicrosize/kg/d Duration: • Tinea pedis, Tinea cruris, tinea manuum, tinea corporis etc. for 2: 6 weeks • Tinea capitis for at least 6: 8 weeks (longer for M canis) • Tinea unguium for 12: 18 months until all signs of nail infection have gone Drug interactions • H2 antagonists should not be taken for 2 hours after griseofulvin because they might otherwise stop its absorption • Griseofulvin reduces the action of: – Warfarin – Oral contraceptives (increasing the chance of pregnancy) Side effects • Headaches • Gastrointestinal upset • Rashes including urticaria,LE • Urinary frequency, bed wetting • Blurred vision, dizziness, depression • Menstrual disturbance • Liver disturbance • Males should not father children within 6 months of treatment with griseofulvin as it may damage sperm cells • C - Safety for use during pregnancy: has not been established.It was found to be teratogenic to pregnant rats; therefore, so should not be prescribed for women contemplating pregnancy Terbinafine (Lamisil ®, Turbin ® 125, 250 mg) • It is an allylamine medicine • It inhibits a fungal enzyme, squalene epoxidase, and stops the cells making ergosterol, the main component of the cell wall • It is absorbed well, with or without food • It may persist in the skin for up to 8 weeks after the drug has been discontinued and in the nails for up to a year Dose regimen • The oral dose for adults is 250 mg daily • For children: – Weight 10-20 kg, 62.5 mg per day – Weight 20-40 kg, 125 mg per day – Weight >40 kg, 250 mg per day • Duration • Tinea corporis, tinea cruris, tinea pedis, tinea manuum: 1 to 4 weeks • Tinea unguium: for 6-8 weeks (fingernails) or 3-4 months (toenails) Side effects • GIT: Nausea, feeling of fullness, diarrhoea, abdominal pain, taste disturbance, loss of appetite • Headache • Dizziness • Abnormal liver function tests • Reduced neutrophil white blood cell count • Allergic skin rash including urticaria and erythema multiforme major (toxic epidermal necrolysis) • Terbinafine should not be taken in pregnancy or during breast-feeding • Terbinafine does not generally alter the concentration of other medications Broad spectrum antifungals (Azoles) Ketoconazole (Nizoral,Kizole,200 mg tab) • Ketoconazole was introduced in 1981 • It is a broad-spectrum synthetic antifungal • Its use has now been limited because other drugs available are less hepatotoxic • It binds to the fungal p450 enzymes and stops the cells making ergosterol, the main component of the cell wall • It is better absorbed orally when it is taken with a fatty meal or acidic drink (e.g. orange juice) • It takes three to ten hours for half of the medication to be cleared from the blood stream • It reaches the surface of the skin through normal blood circulation, sweat and sebum in very high concentrations Dose regimen • In adults is 200 - 400 mg daily are • The dose in children is usually 50 mg per day for those weighing less than 20 kg and 100mg daily for those 20-40 kg Duration • Taken for two to eight weeks • A single dose may be effective for pityriasis versicolor • Nail infections are treated for up to twelve months Side effects • Hepatotoxicity is reported to occur in 1 of 12,000 patients • Abnormal liver function tests (15%) • The main side effects are gastro-intestinal and occur in 5-10% of patients • Testosterone gynecomastia • C - Safety for use during pregnancy has not been established • Although only excreted in tiny amounts from breast milk, it should only be taken by a breastfeeding mother if essential Drug interactions • As ketoconazole needs acid for its absorption, antacids, H2 antagonists should not be taken for 2 hours after it • Ketoconazole may increase the concentration of these drugs and enhance their effect: • Warfarin,methyl prednisolone, ciclosporin, antidiabetic sulphonylurea medication (tolbutamide, glibenclamide, gliclazide, glipizide) • The following drugs markedly decrease the concentration of ketoconazole: Rifampicin, isoniazid, phenytoin Ketoconazole is not thought to interact with the oral contraceptive pill Itraconazole (Sporanox, Itrapex, 100 mg) • Mode of action :Like ketokonazole • The medication is better absorbed orally when it is taken with a fatty meal or acidic drink (e.g. orange juice) • It is bound to proteins such as albumin in the circulating blood and becomes concentrated in fat cells and within skin and nails • It takes one to three days for half of the medication to be cleared from the blood stream • Skin concentrations may be 3 to 10-fold higher than those in the blood. It may persist in the skin for up to 4 weeks after the drug has been discontinued and in the nails for up to a year Dose regimen • Tinea corporis, tinea cruris , tinea pedis, tinea manuum : 200 mg daily for one week OR 100mg daily for 2 weeks • Vulvovaginal candidiasis: 200 mg twice daily for one day OR 200 mg daily for 3 days • Oral candidiasis: 100 mg daily for two weeks • Tinea unguium: 200 mg/day for 6-8 weeks (fingernails) or 3-4 months (toenails), OR 200 mg twice daily for 7 days, repeated monthly for 2 months (fingernails) or 3-4 months (toenails) Side effects • Nausea, vomiting and constipation (5%) • Headache • Abnormal liver function tests (up to 5% for those on long term therapy, 2% for pulse therapy); significant liver disease is rare • Allergic skin rash including urticaria • Endocrine effects gynecomastia • Should be used with caution in those with heart problems • Itraconazole should not be taken in pregnancy. Although only excreted in tiny amounts from breast milk, it should only be taken by a breast-feeding mother if essential Drug interactions • The dose of these drugs should be reduced: – Warfarin – Digoxin – Methyl prednisolone – Ciclosporin – Tacrolimus • The dose of these drugs may need reducing if side effects arise: – Quinidine – Calcium channel blockers – Antidiabetic sulphonylurea medication (tolbutamide, glibenclamide, gliclazide, glipizide) • The following drugs decrease the concentration of itraconazole: – – – – Rifampicin Isoniazid Phenytoin Carbamazepine • Itraconazole is not thought to interact with the oral contraceptive pills Fluconazole (Difflucan, Flucoral, 50 & 150 mg cap) • Fluconazole binds to the fungal p450 enzymes and stops the cells making ergosterol, the main component of the cell wall • Oral absorption is not altered by gastric pH. It takes 22 to 30 hours for half of the medication to be cleared from the blood stream and may take several days of continuous treatment to reach a steady concentration • The drug is eliminated unchanged in the urine so doses should be reduced if there is kidney disease Drug interactions • As itraconazole Side effects • As itraconazole Dose regimen • For vulvovaginal candidiasis, a single oral dose of fluconazole 150 mg is usually effective. It can be repeated • For dermatophyte infections and pityriasis versicolor, either 50 mg daily or 150 mg once weekly is taken for two to six weeks • Larger doses (up to 400 mg daily) are required for systemic infections. • Fluconazole is not normally used in children but doses of 5 mg/kg/day have been safely prescribed for serious infection 2-Topical antifungals • They are applied to the affected area twice daily • For two to four weeks and continued for one or two weeks after the last visible rash has cleared • Including a margin of several centimetres of normal skin • Repeated treatment is often necessary Types I- Azoles They inhibit synthesis of ergosterol,which is necessary for the formation of fungal cell membranes. They are fungistatic • • • • • • Clotrimazole (Canesten, Dermatine) Miconazole (Daktarin, Miconaz) Tioconazole (Trosyd, Tiocon) Ketoconazole (Nizoral, Ketoderm) Econazole (Pevaryl, ecoderm) Seratoconazole (Dermofix) II- Allylamines These also act by inhibiting the formation of ergosterol but block synthesis at an earlier stage in the pathway than imidazoles, namely between squalene and squalene epoxide • Terbinafine (Lamisil, Terbin) • Naftifine )Exoderil) III- Others • Ciclopirox (Batrafen) • Whitefield ointment (Salicylic acid3% Benzoic acid 6%( • Tolnaftate (Tinea cure)