Clinical skills viewed as worthless without communication
advertisement
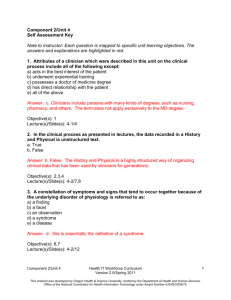
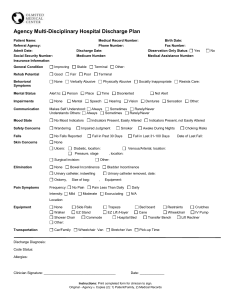
THE FOLLOWING LECTURE HAS BEEN APPROVED FOR ALL STUDENTS This lecture may contain information, ideas, concepts and discursive anecdotes that may be thought provoking and challenging Any issues raised in the lecture may require the viewer to engage in further thought, insight, reflection or critical evaluation Clinical Communication Professor Craig Jackson Prof. Occupational Health Psychology Head of Psychology BCU Clinical Communications Outline Benefits for clients Benefits for clinicians Demerits Skills Shut up and listen Clinical Communications Outline “The good clinician treats the disease, but the great clinician treats the patient” William Osler Relatively new area Communication was a “wet skill” Now part of curriculum Seen as important ( not more important than clinical skill) . . . . . . Clinical skills viewed as worthless without communication Communication skills not universal Different types of communication Depends on therapists’ Training Philosophy inclination Theoretical position Psychodrama Holotropic breathwork CBT RET “Hello Chris” Covert naturalistic experiment 8 sessions with psychotherapist Was NOT psychotherapy Pseudo hypnotherapy Distractions . . . . . iPad Not the “breathy voice” again Sounds too “American” . . . Too controlled . . . Too therapeutic . . . Too effortful . . . Not naturalistic Benefits for Clinicians & Clients Time saving Effective & efficient Reduces Stress & Burnout Reduces litigation Clients more satisfied Best predictor of resolution (e.g. Chronic headache; Headache study group Ontario (1986) Shorter care needed (coronary care patients with emotional support - 2 days less bed time) Mumford et al 1982 Benefits for Clients Positive evaluations Both Clinician and Client agree on reason for consultation Clinician asks client about ideas, concerns or health beliefs Clinician takes time to achieve a shared understanding with client Positive consultations take no longer than negative ones (Arborelius & Bremberg 1992) Improved outcomes A Meeting of Experts Any clinical consultation is a meeting of two experts Clinician - Skills & Knowledge Client - Their body & Experience But sometimes, people just want to be told what to do . . . It’s all subjective of course Clients rating their clinicians Not knowledge based Not skills based Based on communication and subtle cues They might be wrong . . . but their perception is everything Medspeak Jargon Sets boundaries - reminds of power relationships “Sick” “Nerves” “Chronic” “Acute” “Diet” “Drugs” “Stomach” “History“ Lay person Clinician Illness Anxiety Severe Severe Calorie restriction Narcotics Abdomen The past Vomit Neurology Long duration Sudden onset Intake Medication Organ Previous disease Interruptions & Redirections Consultations start with client Appearing rushed Checking watch Fidgeting Monitoring email 28% of clinicians interrupt client in first opening Mean of 23 seconds (Marvel et al 1999) Average of 2 interruptions per consultation Mean of 12 seconds in home consultations (Rhoades et al 2001) Valerie: HIV patient in 1985 Useful sources 90% of info comes from taking a history 10% (or less) from case files and records Visual metaphor Might come in bits and pieces Communication Skills: General Manner 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Responds to cues Active Listening Use Empathy Offer Support Non-judgemental Avoid personal beliefs Simple language Use appropriate body language Questioning style Information giving Information gathering Information Gathering Appropriate language Ordered and Methodological Comprehensive / Succinct Coaxing Use triangulation . . . “So you said that . . . Therefore . . .” Offer partners or collaborators to input Props e.g. clipboard, notes, questionnaire Information Gathering . . . Don’t rely on symptoms “Doorknob concerns” “By the Way” syndrome (Robinson 2001) Clients often reveal real reason only when comfy Real reason is not the first reason hey give Psychosocial issues Worries about future Their own ideas Social context of their problem Barry et al 2000 Information Giving Convey info Check understanding Control of consultation (allows it to vary) Signpost change of direction Summarises / indicates next steps Recognise and respond to client’s concerns and anxieties Consultation General Skills 1. 2. 3. 4. 5. Gives name and explains role; checks patient’s name Gives greeting appropriate to culture (handshake not always needed) Non-verbal behaviour appropriate to culture (eyes not always needed) Establishes purpose of interview Clarifies why interview is taking place: - from client’s perspective - from clinician’s perspective 6. Checks that patient is happy to proceed 7. Establishes desired outcome of interview 8. Establishes baseline knowledge/understanding 9. Uses open questions 10.Listens 11.Confirms what s/he has learned 12.Signals move to information-giving at end Some natural cynicism from medical circles Case Summary of a counselling client Date Symptoms Referral Investigation Outcome 1980 (18) Abdominal pain GP --> surgical OP Appendictomy Normal 1983 (21) Pregnancy (boyfriend in prison) GP --> obs and gynae OP 1985-7 (23-25) Bloating, abdominal blackouts (divorce) GP --> Gastro and neurology OP 1989 (27) Pelvic pain (wants sterilisation) GP --> obs and gynae Sterilised OP Pain persists for 2 years 1991 (29) Fatigue GP --> infectious diseases unit Diagnosis of ME by patient and self help group 1993 (31) Aching muscles GP --> rheumatology Mild cervical clinic spondylosis 1995 (34) Chest pain, breathless A&E --> chest clinic (child truanting) Termination All tests normal Nothing abnormal IBS diagnosis unexplained syncope Pain clinic - Tryptizol Nothing abnormal Refer to psychiatric services poss hyperventilation Summary Clinicians expected to be good communicators Clinical skill does not make up for communication lacking Communication does not replace clinical skills Getting it right worthwhile Rewards Getting it right takes time and experience Clinical supervision essential Case reviews essential Communication without Knowledge Communication without Knowledge Some References Makoul, G. (2001). Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Academic Medicine, 76(4): 390-393. RSM forum on Communication in Healthcare (2004). Core curriculum for communication skills in medical schools. In E. McDonald (ed). Difficult Conversations in Medicine. Oxford: Oxford University Press. pp 209-211. Simpson, M et al. (1991). Doctor-patient communication: the Toronto consensus statement. British Medical Journal. 303(6814): 1385-1387. Von Fragstein, M. et al. (2008) UK consensus statement on the content of communication curricula in undergraduate medicine education. Medical Education 42(11): 1100-1107.