Progress note training
advertisement
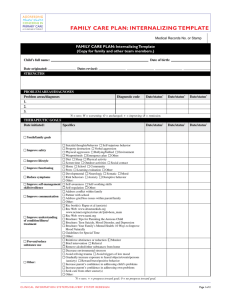
“The Basics You Need to Know” Leave nothing blank on the left side of the form that you are required to fill out ◦ A blank space means you “Forgot” to complete that data entry Leaves the reviewer to guess at the information Always sign, date, and use your credentials (no abbreviations) ◦ Example: John Doe, MS, Senior Community Mental Health Practitioner Progress notes need to be dated the day the session was provided, NOT the day it was written ◦ It is advisable to write your note within 24 hours of the session as to not forget pertinent information Type your notes ◦ ◦ ◦ ◦ ◦ It is more legible Write notes as a single paragraph Do not leave spaces at the end of a sentence or skip line. Check for spelling and grammatical errors Draw a line from the last emptied line to the bottom of the page This prevents someone from “adding” to your note Use proper correction techniques You will need to know your treatment goals and objectives to write your progress note ◦ Single line thru with initial and date above ◦ Be careful with dates… best to re-write the note if your date and time is incorrect ◦ NO WHITE OUT ◦ For your progress note to be billable it MUST be directly related to treatment provided that is based on your treatment plan goals and objectives. ◦ In the event you identify a new problem that is not on your treatment plan or review, make a note in your progress note that “new objective (or goal) has been identified today and you be added to the treatment plan. The new objective (or goal) is as follows…” When a new objective or goal is being added, either a treatment plan review or addendum needs to be completed. The decision as to which document is completed is to be made during supervisor with the Clinical Director Only your client’s name can be identified in your progress note ◦ Confidentiality is an issue for non-clients as well. Siblings, parents, family, etc. names cannot be in your note. ◦ Use descriptive language i.e. John’s youngest sister…. The progress note must describe what the client has done in the session (not what the clinician has done) ◦ Remember this is a note to document details about how treatment is or is not progressing with the client; progress/lack of progress is based on the client and how they are proceeding through treatment. The only section in the note that defines what the clinician did is the Treatment Intervention section. That section will look like “Cognitive Behavioral Treatment”, “Solution Focused,” Play therapy techniques”, etc. A good note uses the FPS “FAIRS format A quality note can be described as: ◦ Clear: good connection between the narrative; treatment goals and objectives; and the interventions ◦ Profession: no spelling or grammatical errors ◦ Has a good use of clinical language ◦ Legible ◦ Informative: Paints a picture of the session ◦ Describes progress of the specific goal and objective addressed that day Your progress notes should not be word for word the same from prior progress notes. Doing this is Medicaid Fraud and can lead to serious repercussions When ever in doubt consult with your Supervisor Clinicians should document EVERY encounter or attempt at an encounter with your client and/or family ◦ No documentation means it NEVER occurred Need to document all your attempts to provide the service ◦ Does not follow FAIRS format ◦ Need to indicate the purpose of the note: Document a telephone call Examples: Attempted to contact: “Clinician left a message stating..” Completed call: Indicate the details of the conversation and the outcome Document a missed session Examples “Clinician canceled due to…” “Client canceled due to…” Progress note A notes: ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ Progress note B notes: ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ F : Focus (Goal & Objectives) A : Assessment (Appearance/ Mood/Etc) I: Intervention (Clinical terminology only) R: Response (Describes session & Progress) Subsequent Plan: (Frequency of session; goals plan to address, etc.) Ensures that you identify the goal(s) and objective(s) you are addressing in the first line of your progress note Prompts you to write/indicate the intervention(s) that you choose to use Prompts you to write the client’s response to treatment and provide detail in how you used your intervention to address the specific goal(s) and objective(s) Identifies the goal(s) and objective (s) you addressed during the current session. Example: Goal: Improve overall mood Objective: Peter will identify 5 triggers that lead to thoughts of hurting himself… Can write in an abbreviated fashion like this: “Goal 1b: Improve mood; id triggers to thoughts of harm” You will practice writing goals & objectives from your treatment plan/review following FAIRS Generalized Anxiety D/O (15 yo female; removed-foster home) ◦ Goal 2: “I don’t want to feel anxious all day” (increased mood stability) Objective d: Nancy will identify at least 3 triggers of fear response… ◦ Rewrite: F)_____________________________________________________ _______________________________________________________ _______________________________________________________. Conduct D/O, childhood onset (6yo maleintact family) ◦ Goal 1: “I want to stop getting in trouble” (Increased compliance) Objective c: Peter will comply with directions with no more than 1 prompt from adult… ◦ Re-write: F) __________________________________________________ __________________________________________________ __________________________________________________. Describes how the client presented during the session Appearance- Physical presentation of client Affect- behavior that expresses an emotion that changes alone with current emotional states and situation 9as compared to mood which describes emotion occurring over a long period of time) Mood- A pervasive and sustained emotion that colors the perception of the world. (In contrast to affect, which refers to more fluctuating changes in emotional ‘weather” mood refers to a more pervasive and sustained emotional “climate”) Behaviors- describe client’s willingness to cooperate or resist clinician during the session Speech- describes communication style used during therapy sessions. You will practice here by describing a client’s presentation in a session using the FAIRS format. ◦ Client is diagnosed with Generalized Anxiety D/O, 15 yo female; and is recently reunited with bio mother after 3 years in a foster home. 1. Choose 2 or more descriptive words for each using the handout provided: ◦ ◦ ◦ ◦ ◦ Appearance: ____________________________ Affect: __________________________________ Behavior:________________________________ Mood: __________________________________ Speech: _________________________________ 2. Write your description of client in a narrative format using 1 to 3 sentences. ◦ A) : _________________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ ________________________________________________________________________. Therapeutic technique- identifies specific therapeutic intervention (s) utilized during current session. The technique must be one of the evidence-based practices Only use if you are familiar with the technique Self-educate to increase your knowledge of different interventions ◦ Reframe from using only 1 type of intervention throughout the course of tx. ◦ Need to use best interventions suited to treat the individual and the issues One of the biggest flaws observed in a progress note is the incorrect use of a therapeutic technique ◦ Your progress note is not billable if your note shows that you are not familiar with how to implement the technique you choose. Elements of the RESPONSE section: ◦ Descriptive narrative Highlights clinical information as it relates back to the current treatment plan goal and objectives being addressed. ◦ Client- Centered Reflects what client is/has done during session (not what clinician is doing). Incorrect: Clinician will complete worksheet with client Correct: Mark will complete worksheet with clinician ◦ Progress Addresses progress on specific objective(s) regularly (at least twice per month; every session best practice) Future: Goal & Objective you plan to address during next session Example: “Continue to meet with David 2x per week for intensive services. Review homework assigned (see note for details of assignment).” CONGRATULATIONS!!!!!!! You have successfully completed the INTRODUCTION TO PROGRESS NOTE WRITING Workshop