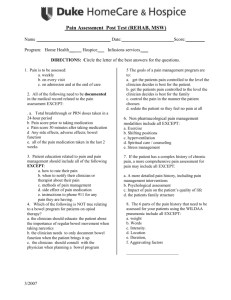
Form - Agency Multi-Disciplinary Hospital Discharge Plan
advertisement
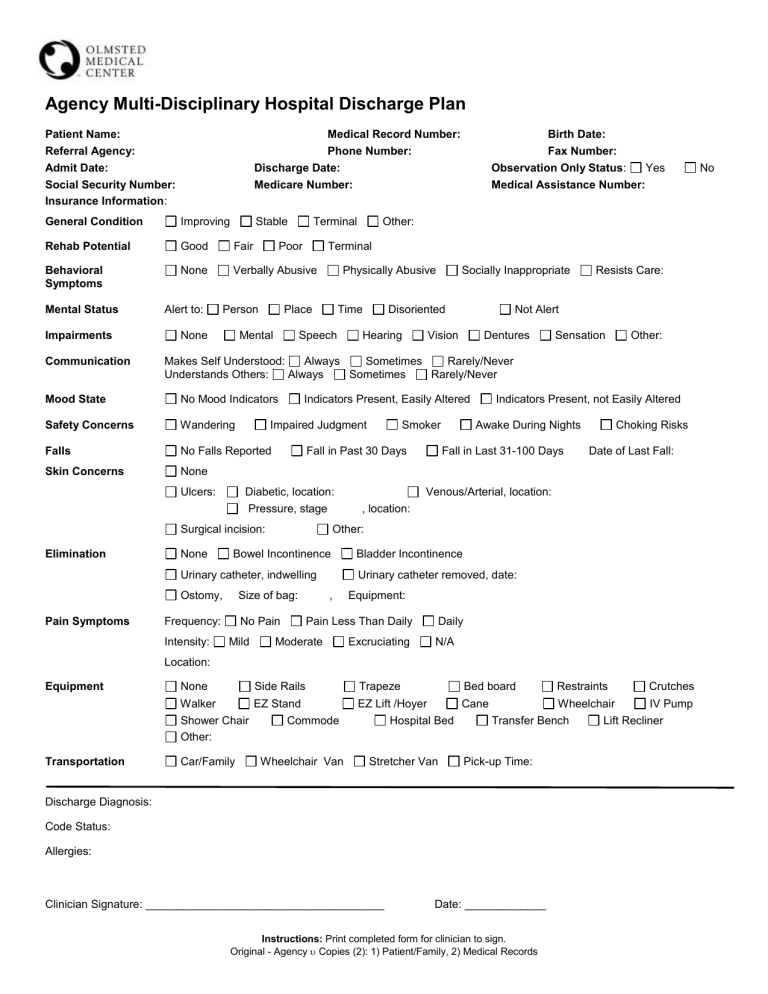
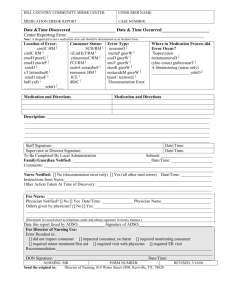
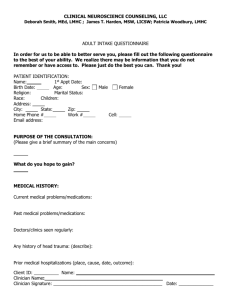
Agency Multi-Disciplinary Hospital Discharge Plan Patient Name: Referral Agency: Admit Date: Social Security Number: Insurance Information: Medical Record Number: Phone Number: Discharge Date: Medicare Number: General Condition Improving Rehab Potential Good Fair Behavioral Symptoms None Verbally Abusive Mental Status Impairments Communication Alert to: Stable Poor Person None Terminal Physically Abusive Time Speech No Mood Indicators Safety Concerns Wandering Falls No Falls Reported Skin Concerns None Ulcers: Disoriented Hearing Resists Care: Not Alert Vision Dentures Indicators Present, Easily Altered Impaired Judgment None Diabetic, location: Pressure, stage Sensation Other: Urinary catheter, indwelling Size of bag: Frequency: Intensity: No Pain Mild Indicators Present, not Easily Altered Awake During Nights Fall in Last 31-100 Days Choking Risks Date of Last Fall: Venous/Arterial, location: , location: Other: Bowel Incontinence Ostomy, Smoker Fall in Past 30 Days Surgical incision: Pain Symptoms Socially Inappropriate Makes Self Understood: Always Sometimes Rarely/Never Understands Others: Always Sometimes Rarely/Never Mood State Elimination Other: Terminal Place Mental Birth Date: Fax Number: Observation Only Status: Yes Medical Assistance Number: Bladder Incontinence Urinary catheter removed, date: , Equipment: Pain Less Than Daily Moderate Excruciating Daily N/A Location: Equipment None Side Rails Walker EZ Stand Shower Chair Commode Other: Transportation Car/Family Wheelchair Van Trapeze Bed board Restraints Crutches EZ Lift /Hoyer Cane Wheelchair IV Pump Hospital Bed Transfer Bench Lift Recliner Stretcher Van Pick-up Time: Discharge Diagnosis: Code Status: Allergies: Clinician Signature: ______________________________________ Date: _____________ Instructions: Print completed form for clinician to sign. Original - Agency Copies (2): 1) Patient/Family, 2) Medical Records No Patient Name: ______________________________________________ Preadmission Screening Complete: Expected Length of Stay: N/A 30 days or less MR#: __________________ DOB: ________________ Yes, Date: N/A Behavioral Health Concerns: Diet: Tube Feeding, formula: rate: Social Information/Patient Preferences: Advance Directive: Legal Oversight: None Power of Attorney: Guardian: Conservator: Healthcare Agent: Contact Person(s): Patient Notified of Healthcare and Discharge Plans: Yes Family Notified of Healthcare and Discharge Plans: Yes, who: Therapy Orders: Physical Therapy No, reason: Occupational Therapy No, reason: Speech Therapy None Physical/Occupational Therapy Summary: Standing Orders: Level of Care: Yes No Skilled Intermediate Home Health Service Clinician Responsible for Care: Clinician Notified: Hospice Yes No, because: Nurse to Complete The Following Activities of Daily Living Code: 0 = Independent 1 = Supervision 2 = Limited Assist 3 = Extensive Assist 4 = Total Dependence Bed Mobility: Transfer: Ambulation: Dressing: Eating: Toilet Use: Personal Hygiene: Bathing: Last Bowel Movement: Treatment Orders: Wound Care: N/A Medication Orders: Yes, specify: See Patient’s Medication List Clinician Signature: ______________________________ 2020407 rev0411 Date: _____________ Instructions: Print completed form for clinician to sign. Original - Agency Copies (2): 1) Patient/Family, 2) Medical Records 5 = N/A Patient Name: ______________________________________________ Medications Given Today and Time: Vaccines, Tetanus: MR#: __________________ DOB: ________________ See Patient’s Medication Administration Record Pneumonia: Flu: Mantoux: Other: Herpes Zoster Vaccine: If greater than 60 years of age, discuss vaccination with primary care provider. Height: Infections: Other: Oxygen: Weight: No No Methicillin Resistant Staphylococcus Aureus (MRSA) Vancomycin Resistant Enterococcus (VRE) Yes, Date Oxygen Last Used: Intravenous (IV) Used: ; No Used at home, name of agency: Yes, for days; Date last dose given: Follow-Up Appointments: Follow-Up Ancillary Testing: Follow-Up Contact Information: Medical/Surgical Department – 507.529.6800 Nurse to Nurse Report given by: OMC Nurse to Facility/Agency Nurse Clinician Signature: ______________________________ 2020407 rev0411 Date: _____________ Instructions: Print completed form for clinician to sign. Original - Agency Copies (2): 1) Patient/Family, 2) Medical Records