Pediatric Toxicology
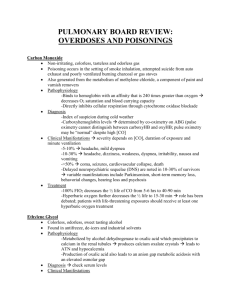
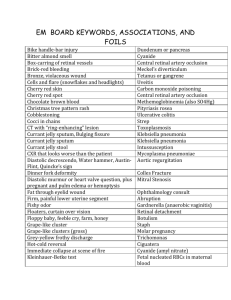
advertisement

Pediatric Toxicology Jana Stockwell, MD Epidemiology 2 million calls 52% of poison center calls <6years Peak ages: 18 months - 3 years Epidemiology Unintentional (1-2 years) – Exploratory – Boys > girls – Unable to discriminate safe from unsafe liquid Intentional (adolescent) – Purposeful – Girls > boys Epidemiology Around meal time Grandparents home Kerosene or gasoline in a soda bottle Older sibling can pharmaceutically treat younger sibling Most often reported Cleaning products Analgesics Cosmetics Cough & cold preparation Insecticides 10% 10% 9% 5% 4% PICU Admission Tricyclic antidepressants (TCA) Anticonvulsants Digoxin Opiates Hydrocarbon-based household products Toxic Exposures Death Analgesics Sedative-hypnotics Alcohols Gases & fumes Cleaning substances “Fatal Sip” Camphor (Vick’s VapoRub) – (100mg/kg) Methyl salicylate (wintergreen) – (200 mg/kg) Benzocaine (OraGel) – 2 mL – Met-hemoglobinemia – Seizure 1000 mg/5 ml 1400 mg/ml “Malignant Swallow” Chloroquine Theophylline Imipramine Chlorpromazine Clonidine – Bradycardia – CNS depression (20 mg/kg) (8.4 mg/kg) (15 mg/kg) (25 mg/kg) (0.3 mg tablet) Other Highly Toxic Acetonitrile - nail tip remover MetHgb Ammonium fluoride – hub cap cleaner (ArmorAll) sz, arrhythmias, acidosis Pennyroyal Oil – some herbal teas Look-Alike, Sound-A-Like Albuterol Celebrex Oruvail Lamictal Lotrimin Plendil Hydralazine Hydrocodone Atenolol Cerebrex Elavil Lomotil Lotensin Pindolol Hydroxyzine Hydrocortisone Poison plants Digitalis effects – Lily-of-the-valley, Foxglove, Oleander, Yew Nicotinic effects – Poison hemlock Atropinic effects – Jimson weed Non-Toxic Products Ball point ink Bubble bath soaps Chalk Cigarettes (< 3 butts) Crayons Deodorants Lipstick Pencil (graphite) Toothpaste Water colors Candle wax (but candle oil is!) Evaluation History of poisoning Physical examination Laboratory studies Gastrointestinal decontamination History What? When? How much? Reliability… What ? Medication Illicit drug Hazardous chemical What form? Pill Solid Liquid Gaseous What route ? Ingestion Inhalation Topical Intravenous When ? Elapsed time How much ? Estimate amount Concentration “Clues” Bradycardia Calcium channel blockers Digoxin Narcotics Organophosphates Carbon monoxide Beta-blockers Clonidine Tachycardia Amphetamine (Ritalin) Atropine TCA’s Theophylline Salicylates (aspirin) Iron Cocaine PCP Synthroid Slow Respiration Alcohol Narcotics Clonidine Sedatives Tachypnea Amphetamines Salicylates Carbon monoxide Ethylene glycol (anti-freeze) Hypotension Calcium channel blockers Carbon monoxide Cyanide Iron Narcotics Anti-hypertensives Met-hemoglobin Hypertension OTC cold remedies Amphetamine PCP TCA Cocaine Diet pills V Tach Amphetamines Carbamzepine (Tegretol) Chloral hydrate Cocaine Digitalis Theophylline Torsades de Pointes Chloral hydrate Cisapride Organophosphates Terfenadine Phenothiazines Hypoglycemia (HOBBIES) Hypoglycemia Oral hypoglycemic agents Beta-Blockers Insulin Ethanol Salicylates Hypothermia Ethanol Narcotics Carbon monoxide Clonidine Hyperpyrexia Atropine Salicylates Theophylline Cocaine TCA CNS - Coma Narcotic Anti-cholinergics Carbon monoxide CNS - Delirium / Psychosis Alcohol PCP / marijuana LSD CNS - Seizure Cocaine Amphetamine Lead Salicylate Isoniazid Theophylline Pupils - Miosis (COPS) Cholinergics, Clonidine Opiates, Organophosphates Phenothiazine, Pilocarpine Sedatives (barbiturates, ethanol) Pupils - Mydriasis (AAAS) Anti-histamine Anti-depressant Anticholinergics (atropine) Sympathomimetics – amphetamine, cocaine, PCP Caution! Polydrug overdoses with opposite pupillary actions Non-toxin diagnoses – Head trauma – CNS hemorrhage Cyanosis MetHgb – Unresponsive to O2 Aniline dyes Nitrites Benzocaine Dapsone Dry Skin Anticholinergic Breath Odors Arsenic Camphor Cyanide Methyl salicylate Paraldehyde Hemlock Garlic Mothballs Bitter almond Wintergreen Pears Carrots Cholinergic “DUMBBELS” “SLUDGE” Example – Organophosphates Nerve agents DUMBBELS Diarrhea, diaphoresis Urination Miosis, muscle fasiculation Bradycardia Bronchospasm Emesis Lacrimation Salivation SLUDGE Salivation Lacrimation Urination Diarrhea GI complaint Emesis Anti-cholinergic syndrome Dry mouth Flushed appearance Dilated pupils Fever Ileus Urinary retention Disorientation Examples – Anti-histamines Jimson weed Lomotil TCA Carbamazepine Glycopyrrolate Atropine Anti-cholinergic Hot as a hare Blind as a bat Dry as a bone Red as a beet Mad as a hatter Full as a flask Narcotic Pinpoint pupils Coma Respiratory depression Salicylates Fever Tachypnea & hyperpnea Lethargy Metabolic acidosis Theophylline Protracted Vomiting Tremors Tachycardia Seizures Hypotension Isoniazid Seizures Metabolic acidosis Hyperglycemia Phencyclidine (4 Cs) Combative Catatonia Convulsion Coma Nystagmus TCA Metabolic acidosis Prolonged QRS Seizures Dilated pupils Dysrhythmia Cyanide Feeling of impending doom Sudden coma Metabolic acidosis Hypotension Bitter almond odor Carbon monoxide Headache Lethargy Dizziness Influenza like syndrome Coma Ethanol Hypoglycemia Lethargy Ataxia Seizure Characteristic breath odor Methanol Severe metabolic acidosis Sluggish pupils Hyperemic retina Blurred vision Ethylene Glycol Lethargy or coma Metabolic acidosis Urinary sediment Crystalluria Clonidine Hypothermia Bradycardia Miosis Respiratory depression Elevated anion gap Methanol Paraldehyde & phenformin Iron & isoniazid Ethylene glycol & ethanol Salicylate ABC’s Airway Breathing Circulation Disability Decontamination Consciousness A: Alert V: Responsive to verbal stimuli P: Responsive to pain U: Unresponsive Drugs Dextrose Oxygen Naloxone Decontamination Ocular- copious saline lavage Skin- copious water GI-consider options Lab Evaluation No “tox panel” that is uniformly helpful Urine Screen Marijuana Amphetamines Barbiturates Cocaine Opiates PCP 5-10 days 48 hours 24 h-2 wks 2-4 days 2 days 8 days EKG All suspected ingestion Tricyclics Pulse oximetry Measure of oxygen saturation of normal hemoglobin Does NOT differentiate CO-Hgb from oxyHgb Falsely low sats – Nail polish – Methylene blue – Poor perfusion Other tests CXR - hydrocarbons ABG - salicylates Esophagoscopy - Caustics Drug levels Acetaminophen Salicylates Methanol Ethylene glycol Iron Theophylline Carbon monoxide (co-ox blood gas) Lithium Radiopaque (CHIPS) Chloral hydrate Heavy metals Iron Phenothiazine (laxatives) Slow release GI tract decontamination Syrup of Ipecac (not used in hospital) Gastric lavage – 1st hour Activated charcoal – Inert – Reduces bioavailability of drug – Not w/ HC or corrosives Cathartics – decrease transit time WBI (whole bowel irrigation)…till clear Urine alkalinization Salicylates Phenobarbital Chlorpropamide Extracorporeal methods Hemodialysis – Severe poisoning – Renal failure Hemoperfusion – Perferred in some toxic ingestions Antidotes Oxygen - carbon monoxide Naloxone – opioids Methylene blue – MetHgb Sodium nitrite - cyanide Deferoxamine – iron Acetoaminophen – N-acetylcysteine Anti-cholinergics – physostigmine Organophosphates – atropine, pralidoxime Benzodiazepines – flumazenil B-blockers – glucagon TCA – bicarb Coumadin – Vitamin K Fomepizole (Antizol) – ethylene glycol