Critical Care Mgmt of Poisonings
advertisement

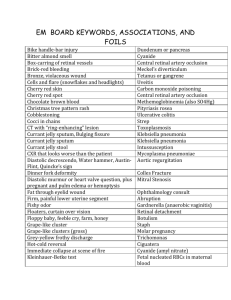
Elliot Melendez, MD Objectives Discuss Principles of Toxin Assessment and Screening Discuss toxidromes and their management Discuss specific toxins I will try not talk about decontamination or elimination of toxins I will not follow Fuhrman word-for-word You should have read the 2 chapters (98,99) Epidemiology > 2 million calls to poison control centers per year ~ 66% involve < 20 years ~ 52% < 6 years Only 25% require referral to a health care facility 1 of 8 require critical care admission Mortality 2.1% < 6 years 8.1% < 20 years Epidemiology Highest incidence in 1-3 year olds (accidental) Boys > girls Children with developmental delay or pica Second peak in adolescents suicide attempt or experimentation Females >>> males Anorexia and psychiatric conditions risk factors Epidemiology Most occur when parents distracted at home 2nd most common site is at grandparents’ homes 91% occur in the home Many involve household products or meds that are left open and being used at the time Pediatric Ingestions (< 6 yrs) Cosmetics Cleaning Analgesics Plants FB Cough/cold Topicals 13.3% 11.0% 7.6% 7.1% 6.3% 5.5% 5.4% Insecticides Vitamins Antimicrobials GI preps Arts/crafts *Hydrocarbons Antihistamines 3.9% 3.3% 3.1% 3.0% 2.5% 2.2% 1.9% Epidemiology Agents involved known in most cases In unknown cases, recognition of a toxic syndrome may help in management Common toxic agents leading to hospitalization Caustics Rx Meds (antidepressants) Analgesics (acetaminophen) Heavy metals (lead) Agents Leading to ICU Rx meds TCA Anticonvulsants Digitalis Opiates Alcohol Hydrocarbon household products Pediatric Pitfalls Suspicious if: Altered mental status Multiple organ dysfunction New onset, afebrile sz Acute onset of presenting sx Hx of previous ingestions Current household stress/pregnancy/visitors Pediatric Pitfalls Difficult Hx: Uncooperative/preverbal patient Abuse Fear of parental discipline Get the bottle! Assessment of Poisoned Patient An accurate history is vitally important. Parents usually minimize the child’s exposure to a toxin in order to deny threat of injury or assuage guilt However, frequently, the precise time and toxin are accurately known. Evaluating for the Unknown Substance History Obtain ingredients in suspected toxins Ask to see containers Assume the worst possible scenario in calculating max dose Use max amt of missing tablets or liquid Concentration of drug or chemical Child’s weight Priorities Assess for medical stability A, B, C, D’s Airway/Breathing – Consider intubation? Upper airway obstruction Excessive bronchial secretions Loss of airway reflexes Respiratory failure Priorities Circulation Assess and treat hypertension and tachycardia ○ Typically if patient is agitated, use sedatives first ○ Avoid non-selective blockers Treat hypotension with fluids first, and if needed, use direct agonists Disability Protect patient from self-harm Treat seizures and protect airway Diagnosis via Toxidromes Why don’t they work? Memorization? Not all clinical criteria may be present Polysubstance ingestion complicates clinical signs and symptoms What Works? Exam And what poison control wants to hear! Vital signs: Temp, HR, BP, RR, Sats Pupil size Skin (dry or wet) Level of Consciousness/Mental status Let’s Work this Through Temperature Fever Sympathomimetics/Anticholinergics ASA Neuroleptic malignant syndrome, MH Hypothermia Depressants Alcohol Barbiturates Let’s Work this Through Heart Rate Tachycardia – Sympathomimetics/Anticholinergics – Antihistamines – TCA – Bradycardia Ca channel and beta blocker, pure alpha agonists Digoxin Opiates/Sedative hypnotics Clonidine Cholinergics/Organophosphates Let’s Work this Through Blood Pressure Hypertension – Clonidine? – Sympathomimetics/Anticholinergics – Trauma, CNS bleed from adrenergics Hypotension Ca channel and beta blocker Barbiturates Opiates Sympatholytics - clonidine Vasodilators/Diuretics Let’s Work this Through RR and O2 sats Respiratory Depression Opiates Barbiturates Respiratory distress ASA (metabolic acidosis) – Sympathomimetics/Anticholinergics – Organophosphates Let’s Work this Through Pupil Size Pupils Small (Miosis) Cholinergics Opiates Clonidine Organophosphates Sedatives/Barbiturates Pupils Dilated (Mydriasis) Sympathomimetics/Anticholinergics Antidepressants (SSRI, TCA) Let’s Work this Through Skin Wet – Sympathomimetics – Organophosphates – Cholinergics Dry Anticholinergics Let’s Work this Through Mental Status Agitated/Confused/Seizures Sympathomimetics/Anticholinergics Withdrawal syndromes Depressed Alcohols Opiates/Barbiturates Sedatives/Hypnotics TCA Laboratory Studies Chem 10 Calculate serum anion gap Pregnancy test EKG Sosm Calculate osmolar gap if alcohol suspect LFTs, Coags Blood gas Urine pH X-rays Laboratory Studies Blood levels useful to assess risk ASA, Tylenol, anticonvulsants, alcohol Tox Screens Only occasionally reveals an unanticipated toxin Most commonly confirms what is suspected from history and exam. Tox Screens Know you institutions screens and their limitations Suboxone, methadone, and dextromethorphan do not show up on urine tox Benadryl, Tegretol cross-react with TCA screen ICU Management Mostly Supportive Very few antidotes Consider “Coma” Cocktail Naloxone Glucose Thiamine Flumazenil Physostigmine Consult with local poison control Specific Cases 16 y/o girl with history of anorexia is brought to ED for confusion, agitation What do you want to know? Case #1 Temp 100.3 HR 130 BP 150/90 RR 20 O2 sat 99% RA What else? Case #1 Pupils dilated, poorly reactive Skin: Dry Mental Status Agitated Paranoid Picking things from air Case #1 Diagnosis? Case #1 Anticholinergic syndrome Drugs: TCA Antihistamines Belladona Others Labs? Labs Chem 7 normal CBC normal Urine tox negative Serum tox negative Tylenol, ASA, TCA, EtOH EKG normal Mother asks, “Could this be from her new appetite stimulant medication.” Management Treat agitation with sedatives as needed Diagnostic test? Diagnostic Test? Physostigmine Ach-ase inhibitor, transient Risks: ○ Seizures ○ Asystole ○ Have atropine available!!!! Case #2 16 y/o girl just broke up with her boyfriend, presents with seizure. What do you want to know? Case #2 Temp 100.3 HR 130 BP 150/90 RR 20 O2 sat 99% RA Seizing What else? Case 2 What do you mean what else? Treat the seizure!!! Ativan, Ativan seizure stops Okay, now what else? Case #2 Pupils dilated, poorly reactive Skin: Dry Mental Status Depressed, intermittent agitation Labs? Labs Chem 7 normal CBC normal Tox screens sent EKG with QRS 0.12 Mother states no meds in home other than her migraine meds Case #2 What do you do next? Case #2 Management Depression ? Migraine medication Seizure Anticholinergic syndrome Tachycardia with QRS >0.1 Case #2 TCA = Tachycardia, Convulsions, Anticholinergic Treatment? Case #2 Treatment Alkalinize the serum!!! NOT THE URINE NaHCO3 IVP until QRS < 0.1 How much? As much as if takes!!! If this symptomatic, start NaHCO3 drip once QRS narrowed, goal pH 7.45-7.55. If nonsymptomatic, NS infusion at 1.5 maintenance, with NaHCO3 at bedside Case #2 Seizes again Ativan doesn’t stop seizures after 2 doses. Next? Case #2 Still Seizing DO NOT GIVE PHENYTOIN Na channel blocker, which is what TCA’s do and can make things worse Continue NaHCO3 push and Ativan, consider pentobarbital, Propofol TCA Toxicity TCAs block Na channels leading to effects Seizures correlated with QRS > 0.1 Arrhythmias with QRS > 0.16 Rarely, prolonged QTc (but not without QRS widening) You don’t have TCA toxicity without tachycardia. If initially asymptomatic, and no symptoms by 6 hrs of ingestion, PICU monitoring not needed. Other Notable Ingestions Serotonin Syndrome Altered MS, Increased muscle activity, clonus, autonomic instability Seen with SSRI overdoses, combination of ingestions leading to serotonin increase ASA Metabolic acidosis, but respiratory alkalosis Alkalinize urine!!! If tinnitus, level > 30. Think of sources other than ASA ○ Bismuth, oil of wintergreen, topical acne meds Summary VS, Pupils, Skin, MS should give you a clue to agent Tox screens rarely helpful Look at AG and Sosm when appropriate