OVERDOSES AND POISONINGS
advertisement

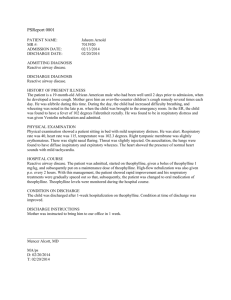
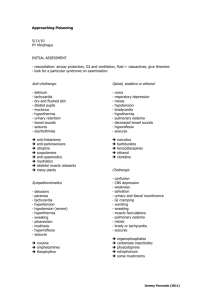
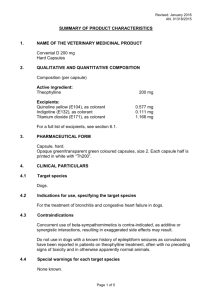
PULMONARY BOARD REVIEW: OVERDOSES AND POISONINGS Carbon Monoxide Non-irritating, colorless, tasteless and odorless gas Poisoning occurs in the setting of smoke inhalation, attempted suicide from auto exhaust and poorly ventilated burning charcoal or gas stoves Also generated from the metabolism of methylene chloride, a component of paint and varnish removers Pathophysiology -Binds to hemoglobin with an affinity that is 240 times greater than oxygen decreases O2 saturation and blood carrying capacity -Directly inhibits cellular respiration through cytochrome oxidase blockade Diagnosis -Index of suspicion during cold weather -Carboxyhemoglobin levels determined by co-oximetry on ABG (pulse oximetry cannot distinguish between carboxyHB and oxyHB; pulse oximetry may be “normal” despite high [CO] Clinical Manifestations severity depends on [CO], duration of exposure and minute ventilation -5-10% headache, mild dyspnea -10-30% headache, dizziness, weakness, dyspnea, irritability, nausea and vomiting ->50% coma, seizures, cardiovascular collapse, death -Delayed neuropsychiatric sequelae (DNS) are noted in 10-30% of survivors variable manifestations include Parkinsonism, short-term memory loss, behavorial changes, hearing loss and psychosis Treatment -100% FIO2 decreases the ½ life of CO from 5-6 hrs to 40-90 min -Hyperbaric oxygen further decreases the ½ life to 15-30 min role has been debated; patients with life-threatening exposures should receive at least one hyperbaric oxygen treatment Ethylene Glycol Colorless, odorless, sweet tasting alcohol Found in antifreeze, de-icers and industrial solvents Pathophysiology -Metabolized by alcohol dehydrogenase to oxalic acid which precipitates to calcium in the renal tubules produces calcium oxalate crystals leads to ATN and hypocalcemia -Production of oxalic acid also leads to an anion gap metabolic acidosis with an elevated osmolar gap Diagnosis check serum levels Clinical Manifestations -Stage 1 (30 min-12 hrs) inebriation, ataxia, seizures -Stage 2 (12 hrs-24 hrs) myocardial dysfunction, pulmonary edema -Stage 3 (2-3 days) acute renal failure Treatment need to inhibit formation of toxic metabolites -Supportive measures Gastric lavage in the first hour post-ingestions, administration of calcium, folate, thiamine and B6 -Ethanol infusion supplied as a 10% solution in D5W containing 10g of ethanol per 100 cc of solution Target level 100-200 mg/dL Loading dose 0.6g/kg Maintainence dose 66 mg/kg/hr (non-alcoholics) 154 mg/kg/hr (alcoholics) -Fomepizole directly inhibits alcohol dehydrogenase Used until toxic levels fall to < 20 Loading dose 15 mg/kg IV Maintenance dose 10 mg/kg IV q 12 -Hemodialysis indications include: Levels > 50 Significant and refractory metabolic acidosis Evidence of end-organ damage Methanol Colorless, odorless, bitter tasting alcohol Found in paint removers, duplicator fluid and windshield washing fluid Pathophysiology -Metabolized by alcohol dehydrogenase to formic acid which leads to visual symptoms secondary to optic nerve swelling -Production of formic acid also leads to an anion gap metabolic acidosis with an elevated osmolar gap Diagnosis check serum levels Clinical Manifestations -Up to 6 hrs headache, dizziness, ataxia, confusion -6 hrs-3 days visual symptoms, acidosis, pancreatitis Treatment same as ethylene glycol -Hemodialysis indications include Levels > 50 Lethal dose ingested Significant and refractory metabolic acidosis Evidence of end-organ damage Isopropanol Colorless, bitter tasting alcohol which smells like acetone Found in rubbing alcohol, skin lotions, hair tonics, aftershave, de-icers Pathophysiology -Metabolized by alcohol dehydrogenase to acetone -Does not lead to anion gap metabolic acidosis Clinical Manifestations -Sweet smelling breath -Urinary ketones -Elevated osmolar gap without metabolic acidosis -Hemorrhagic gastritis Treatment -Gastric lavage if performed within 1 hour of ingestions -Supportive measures are usually sufficient -Hemodialysis indications include Lethal dose ingested Levels >400 Refractory shock Prolonged coma Theophylline Toxicity: 1. Theophylline has a low therapeutic index. The usual recommended therapeutic plasma concentration is 10 to 20 mg/L 2. Theophylline is extensively metabolized by hepatic cytochrome P450, as only a small fraction is excreted in the urine - The half-life of theophylline in a healthy adult nonsmoker averages 8 hours, but increases to 30 hours or more in the presence of chronic liver disease 3. Decreased theophylline clearance - when metabolism of the drug is slowed by the presence of concomitant disease (such as heart failure or liver disease) or by the concurrent administration of other drugs (including erythromycin, cimetidine, ciprofloxacin, cephalexin, tetracycline, birth control pills, allopurinol, propranolol, and thiabendazole). Age above 60 years and early infancy. 4. Clinical: a. Seizures can occur at a plasma theophylline concentration as low as 25 mg/L. They are, however, more common at levels above 40 mg/L and, with chronic dosing, are almost universal above 100 mg/L - The risk is less with an acute OD b. Arrhythmias can begin when the plasma theophylline level is greater than 20 to 30 mg/L, but cardiovascular collapse and respiratory arrest are rare unless the concentration is greater than 50 mg/L with chronic therapy or above 100 mg/L with an acute overdose c. Hypokalemia, hypomagnesemia, hypophosphatemia, hypercalcemia, hyperglycemia, and respiratory alkalosis d. Rhabdomyolysis occurs in selected cases 5. Treatment: a. Decreased intestinal absorption - gastric lavage, activated charcoal given with a cathartic such as sorbitol b. Beta blockers and anti-arrhythmic agents c. Control of seizures – benzo > dilantin d. Renal Replacement Indications: i. If the patient is clinically unstable or has seizures, life-threatening hypotension, and/or arrhythmias ii. If the acutely intoxicated patient has a plasma theophylline concentration above 100 mg/L iii. If a chronically intoxicated patient is over age 60 and has a plasma theophylline level above 40 mg/dL iv. If a younger chronically intoxicated patient has a plasma concentration above 60 mg/L. If the plasma level is just above this value and the patient is stable, dialysis can be delayed for two hours pending a second plasma level in those patients who can tolerate repeated oral charcoal v. If the plasma theophylline level is above 60 mg/L in a patient at high risk for seizures or one or more of the following problems: 1. Impaired metabolism of theophylline due to chronic liver disease, heart failure, or hypoxemia (PO2 40 mmHg). 2. Inability to tolerate repeated dose oral charcoal because of intractable vomiting or intestinal ileus. 3. Increased susceptibility to severe toxicity, which occurs in patients who are elderly or who have ischemic heart disease, severe chronic lung disease, or a history of epilepsy vi. HD = net effect is removal of 40 percent of the administered dose in three hours, added advantage of correcting the electrolyte abnormalities vii. HP = Hemoperfusion is even more effective, HP cartridges are prone to saturation – may have to change the cartridge every two hours Clostridium: 1. Botulinum: a. Food Botulism: i. descending muscle weakness – upper extremities to lower extremities ii. CN – blurred vision, diplopia, ptosis, urinary retention b. Wound Botulism: like food c. D/D: MG (no autonomic findings), LEMS, Tick Paralysis, GBS (ascending paralysis), Polio, CVA d. Think botulism: no fever, symmetrical neurological findings, responsive, normal to decreased heart rate, normal BP, no sensory deficits e. Treatment: Botulism anti-toxin (SE: serum sickness), PCN G or Flagyl 2. Tetani: a. Tetanus toxin blocks neurotransmission disinhibits neuron (ant. Horn cells) increased muscle tone, spasms, autonomic instability b. Clinical: lockjaw, sweating, tachycardia, fever, increased or decreased BP, Aware!, stiff neck, opisthotonus, sardonic smile, rigid abdomen, periods of apnea, dysphagia c. Treatment: i. wound debridement ii. PCN G or Cephalosporin or Flagyl iii. Tetanus immune globulin iv. Active immunization – TD x 3 every 2 weeks v. Benzos, baclofen, b-blocker, MgSO4