QIPP national workstream – briefing paper
Workstream
Workstream Lead
Slide 1 of 4
Right Care
Sir Muir Gray and Philip DaSilva
1. The opportunity
QUALITY Right Care is designed to seize the opportunity provided by the tight financial climate to improve the way
we use resources in the NHS whilst improving health outcomes and patient experience. By focussing on
commissioning care pathways as whole systems instead of commissioning activity from bureaucratic structures and by
collaborating with clinicians, within the context of programme budgets, we can eliminate wasteful spend on low value
activities and focus resources on high value activities, maximising value for the population as a whole. We can also
improve patients’ care and outcomes by ensuring they do not undergo inappropriate or unnecessary interventions.
Right Care will encourage a debate between the public, clinicians and managers in order to achieve a common
agreement about what is high and low value.
The Shared Decision Making project will empower patients to make rational healthcare decisions, based upon a fuller
understanding of the risks and benefits of treatment options. There is clear international evidence that patients, when
supported with decisions aids, increasingly choose less invasive and therefore less costly treatments which result in a
better patient experience and at least as good outcomes as usual care.
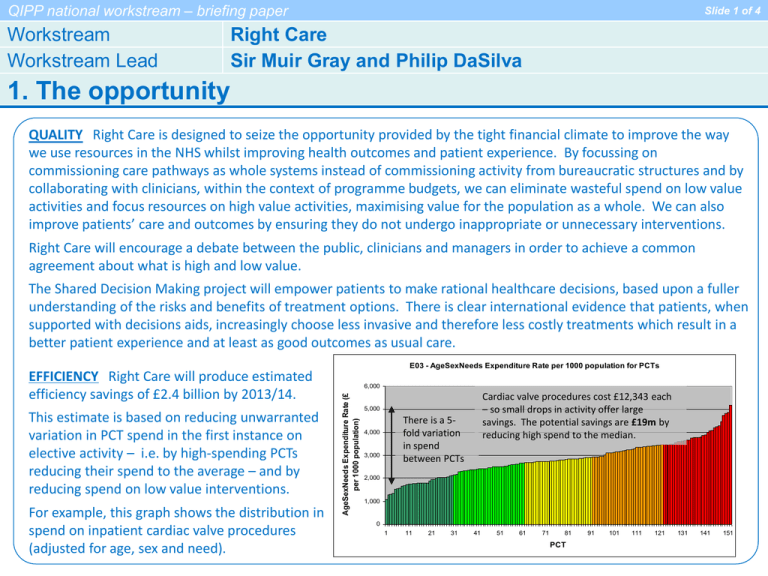
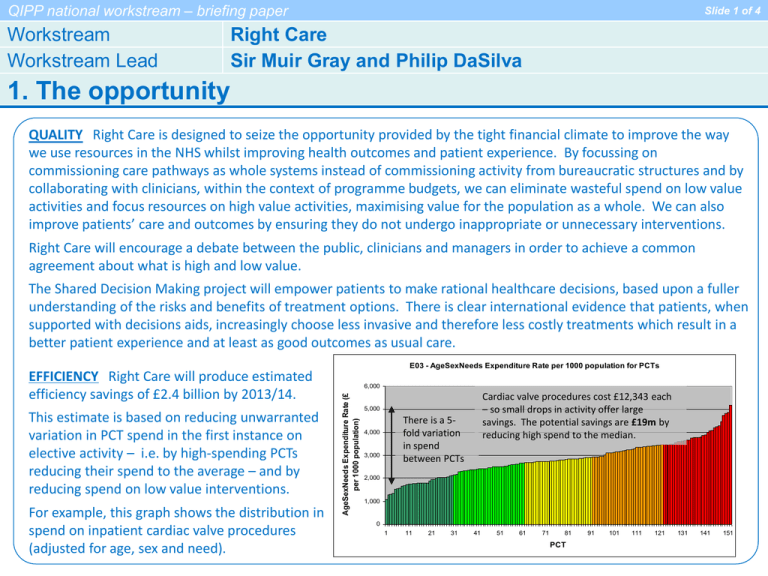
E03 - AgeSexNeeds Expenditure Rate per 1000 population for PCTs
This estimate is based on reducing unwarranted
variation in PCT spend in the first instance on
elective activity – i.e. by high-spending PCTs
reducing their spend to the average – and by
reducing spend on low value interventions.
For example, this graph shows the distribution in
spend on inpatient cardiac valve procedures
(adjusted for age, sex and need).
6,000
AgeSexNeeds Expenditure Rate (£
per 1000 population)
EFFICIENCY Right Care will produce estimated
efficiency savings of £2.4 billion by 2013/14.
Cardiac valve procedures cost £12,343 each
– so small drops in activity offer large
savings. The potential savings are £19m by
reducing high spend to the median.
5,000
There is a 5fold variation
in spend
between PCTs
4,000
3,000
2,000
1,000
0
1
11
21
31
41
51
61
71
81
PCT
91
101
111
121
131
141
151
QIPP national workstream – briefing paper
Workstream
Workstream Lead
Slide 2 of 4
Right Care
Sir Muir Gray and Philip DaSilva
2. The case for change
NHS management has often focussed on organisations and structures. Clinicians have held the balance of power, creating
clinical systems of an ever increasing sophistication. Historically, use of NHS resource has been driven by un-checked
demand, often supported by clinician and health organisational imperatives which have a tendency towards expanding and
providing more services or use of new technology, sometimes without a sound evidence base and with little regard to
ceasing other ways of working or paying much attention to the impact on the health system as a whole. Currently patients
undergo treatment in the face of “avoidable ignorance” and consent to interventions which they would not undergo if they
were provided with a fuller understanding of the risks, benefits and alternatives to fully exercise their values and
preferences.
The ambition of Right Care is to change thinking on commissioning care away from organisations and contracts to
commissioning high value, whole system pathways, under-pinned by networks rather than institutions and putting the
citizen and the patient at the centre of this discussion. Those systems and networks can begin to take on programme
budgetary financial risk and rewards in addition to whole pathway clinical quality accountability. A key component is the
provision of tools and analysis which highlight the often large and unexplained variations in spend on healthcare and health
outcomes for the commissioner’s population.
It is also evident that the public and patients have not always been included in the debate about the development or design
of services. The NHS is unlikely to hold sufficient resource to meet ever rising demand and thus we need to change the
nature of the debate between the public and the NHS about how resources are utilised for their care - to do the right things,
at the right time and place, safely and effectively. This activity will also increase the sustainability of healthcare.
Evidence from the Public Health Commissioning Network shows that clinical networks are cost effective and feasible and
that integrating systems of care are an effective means of delivering value and quality. They can help us to address problems
such as:
• failure to adopt and implement strong evidence;
• massive unknowing duplication of effort in appraising new technologies;
• a lack of focus on common expensive problems such as epilepsy or headache.
QIPP national workstream – briefing paper
Workstream
Workstream Lead
Slide 3 of 4
Right Care
Sir Muir Gray and Philip DaSilva
3. The planned approach
Sir Muir Gray
Chief
Knowledge
Officer of the
NHS, DH
Sir Muir has worked in public health for
35 years. He helped pioneer Britain's
breast and cervical cancer screening
programmes and was knighted in 2005
for the development of the foetal,
maternal and child screening
programme and the creation of the
National Library for Health.
Philip DaSilva
National QIPP
Lead, Primary
& Community
Services
Phil has a nursing background
and brings more than 30 years’
NHS experience to the team,
operating at all levels including
as a PCT Chief Executive and
in a range of senior Executive
Director positions.
WHAT Right Care will create better value programmes and systems of care within programme budget areas by
supporting networks of lead clinicians and commissioners in local health economies to develop and commission high
value pathways for specific clinical programmes.
Right Care will support this work with learning programmes, knowledge management tools and Accelerated Design
Events. It will also support clinical commissioners with a range of tools including the NHS Atlas of Variation, the
Annual Population Value Review, lists of high and low value interventions and the systematic use of the Map of
Medicine and NHS Evidence .
A project on Shared Decision Making, led by East of England SHA, complements and feeds into Right Care. This will
deliver a National Strategy for Shared Decisions and at least six new NHS decision aids on a national platform (see
screenshot).
HOW Right Care will provide the focus, leadership and support to
drive momentum and accelerated change in clinical commissioning,
where improvement is currently recognised to be slow and sporadic.
The work will become core to the review of World Class Commissioning
with the extension and enhancement of WCC competencies.
A small national reference group will advise on using national levers
(e.g. standard contracts, tariff, ring-fenced budgets) to drive change.
QIPP national workstream – briefing paper
Workstream
Workstream Lead
Slide 4 of 4
Right Care
Sir Muir Gray and Philip DaSilva
4. Case study
A team of clinicians and commissioners is using clinical evidence
to redesign the COPD pathway ensuring that access to health
care is improved for patients that will result in fewer
readmissions.
Central lancashire PCT has identified three interventions to
reduce cost on the COPD pathway:
1. Invest in community health care
2. Reduce readmissions
3. Work to reduce length of stay of hospitalised patients
Quality outcome:
This workstream sets out to increase value by improving clinical
commissioning - the right allocation of resources to different
COPD patients receive appropriate care in a community setting
clinical specialties; clinical management - the right use of
and are less likely to need emergency admission to hospital
allocated resources each group of patients; and patient choice Productivity outcome:
to ensure that the patient makes the decision that is right for
them
By redesigning the clinical pathway for COPD and
commissioning more community based care this PCT has an
Central Lancashire PCT is taking this approach to increase the
aspiration to reduce its spend on hospital readmissions for
value it derives from the £34m it allocates for respiratory
COPD patients by £500,000 a year.
disease, initially by improving the quality and health outcomes
of the chronic obstructive pulmonary disease (COPD) service. It
is working to reduce readmission rates by 10% and at the same
time ensure that more people are cared for at home.
In this PCT the COPD spend is £7million a year. This is 17%
more than neighbouring PCTs. The main hospital has a COPD
admission rate of 46% compared with a 27% national admission
rate. Emergency hospital admissions due to exacerbations of
COPD account for 70% of the total costs for COPD patients.
The workstream will work to derive increased value from three
programmes:
•Respiratory disease, current cost £4.27bn a year
•Gastrointestinal and liver disease, current cost £4.10bn a year
•Genito-urinary disease including kidney disease, current cost £4.0bn
The above costs do not count GP costs other than prescribed
medication