LS 3 Storyboard Better Breathing
advertisement
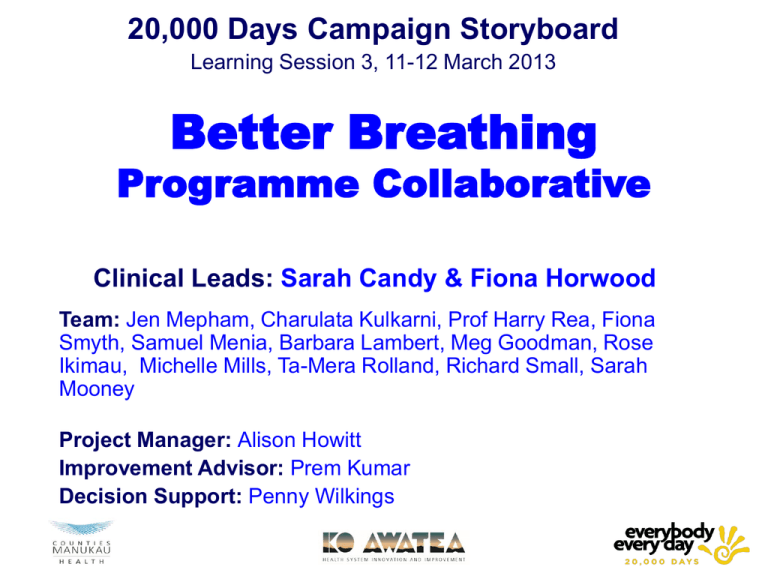
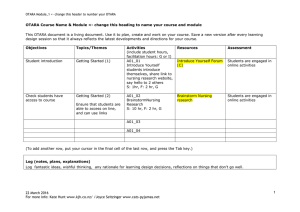
20,000 Days Campaign Storyboard Learning Session 3, 11-12 March 2013 Better Breathing Programme Collaborative Clinical Leads: Sarah Candy & Fiona Horwood Team: Jen Mepham, Charulata Kulkarni, Prof Harry Rea, Fiona Smyth, Samuel Menia, Barbara Lambert, Meg Goodman, Rose Ikimau, Michelle Mills, Ta-Mera Rolland, Richard Small, Sarah Mooney Project Manager: Alison Howitt Improvement Advisor: Prem Kumar Decision Support: Penny Wilkings Aim • The aim of this project is to keep more people with chronic respiratory disease well in the community by increasing the number of participants enrolled into Better Breathing (community based pulmonary rehabilitation) from 60 to 250 per year. This will result in; a reduction of unplanned admissions, increased exercise tolerance and improved health related quality of life. Driver Diagram - Include Collaborative Driver Diagram Change Packages 2O Drivers Change Ideas Tested (describe process) Evidence of Improvement Access & Community Community Location and Venue Transport options Attendance & Feedback Access & Community Patient Engagement GP support and involvement Supporting attendance for Maori and Pacific patients Attendance & Feedback Identifying patients Referrals Assessments Waiting List, drop outs & starting programme (Theory of change) Change Packages 2oDrivers (Theory of change) Change Ideas Tested (describe process) Evidence of Improvement Programme Programme Content Sessions and format Equipment Speakers Clinical outcome assessments Based on current research, modifications based on testing, user feedback. Combined Programme Healthy Hearts – Heart Failure Initial set up phase. Patients Most Successful PDSA Cycles? - Include PDSA Tree diagram Most Successful PDSA? • Continue to refine and measure the programmes. • Offer as a Franchise model with flexibility to suit patient demographice Act • Programmes need to be Study design to suit the community they serve and each community is different. • Having the flexibility to provide programmes tailored to the patient demographics is essential for best outcomes • Additional pulmonary rehabilitation programme into the community • Otara • Pukekohe Plan Do • • • • • • Identify & secure venues Supply equipment Design programme Engage Community Identify patients Arrange staffing & speakers • Start programme Measures Summary • Outcome Measures – The number of patients enrolled in each community Better Breathing programme – The number of unplanned hospital admissions • Process Measures – The number of referrals to Better Breathing – The number of participants who start Better Breathing – The number of participants completing the programme – The change in distance walked on 6 minute walk test – The change in health related quality of life questionnaire scores Implementation Implementation Areas Changes to Support Implementation Standardisation Developing Process Map Programme Guidelines PDSA cycles Developed Otara, To some extent tested in Pukekohe Documentation Plan to create a franchise “options” document giving examples as case studies Training Measurement Resourcing Developing training materials Testing on new staff Produce and monitor guideline measures, covering clinical outcomes, patient drop out and completions targets. Information on ideal venue, staffing and equipment in Franchise document. Adapted from “The Improvement Guide. A Practical Approach to Enhancing Organizational Performance” Gerald Langley et al., 2009, p180. Highlights and Lowlights Highlights - Accessibility – patients report they are now able to attend a programme - Patients feel safe and supported in a familiar environment which is in the heart of their community - As a whole, the pulmonary rehabilitation service is able to offer an increased number places on the programme (240 – 450) - Increased profile of pulmonary rehabilitation in South Auckland Lowlights - Recruitment of staff - Practise nurse involvement in Otara - Pukekohe site size and availability Achievements to date Moving Pulmonary Rehabilitation to the community Venues, equipment, programme, speakers, referrals, assessments, staff, speakers, advertising, patient information, cultural support Starting the Better Breathing Programme in Otara (running for 7 months) Starting the Better Breathing Programme in Pukekohe. (4 intakes) Testing and refining everything while we are doing it. Learning from the patients and the community Co-ordinating all the various groups, departments, stakeholders and people. Thank you to everybody that has been involved 20,000 Days Campaign Storyboard Learning Session 3, 11-12 March 2013 Better Breathing Clinical Pathway Clinical Leads: Fiona Horwood, Richard Hulme Team: Katie Coulter, Nicola Corna, Diana Hart, Sue Beaumont-Orr, Michelle Mills, Ta-Mera Rolland, Richard Small Project Manager: Alison Howitt Improvement Advisor: Prem Kumar Decision Support: Tanesha Patel Aim • The overall aim of the Better Breathing Collaborative is to work together with the Counties Manukau Community to help people with breathing problems to manage their condition well in the community. • This will be accomplished by •Providing community based pulmonary rehabilitation, for 250 in Otara and Pukekohe. •Introducing a COPD care bundle for patients with a primary diagnosis of COPD patients in Middlemore Hospital. •Increasing the numbers of COPD patients, identified in primary care and by piloting the introduction of an “early diagnosis primary care bundle.” Driver Diagram - Include Collaborative Driver Diagram Primary Care Change Packages 2o Drivers Change Ideas Tested Describe Process (Theory of change) Early Primary Care Bundle Diagnosis The receptionist gives a CAT survey to a patient who is 40y+, is a smoker or ex-smoker & doesn’t have known asthma. The CAT survey has been incorporated into a decision support tool in the GP Patient Management System. GP act on the information provided by the patient Clinical Pathway Roll out CME course developed by Clinical Pathway Group and ProCare. Focus on spirometry and WOF. Primary Care COPD Pathway CME Primary and Secondary Change Ideas to be tested 2o Drivers Change Ideas (describe process) (Theory of change) Secondary care bundle has been developed and tested, using the “pink” form Winter warrant of fitness for target patients Options for spirometry in the community • • • • Practices/Shared Group of Practices Locality Hub Alongside Better Breathing Programme Huff and Puff Bus Evidence Further evidence is required Most Successful PDSA Cycles? Based on UK developed Care Bundle Tested Resp Ward Re-think and Simplify Tested Resp Ward Order changed Y/N added Tested Resp Ward One box removed, not enough patients to test Tested Resp Ward & Gen Ward Further info added for non Resp wards Tested on Gen Ward Referral Check box, sign & date added Tested Resp & Gen Ward Testing continues and we’ve learn’t a lot Measures Summary - Measures related to Aim Graphs of key measures Which of your run charts would you give to senior leadership to use? Include Collaborative Dashboard Measures Summary Outcome Measure • Unplanned admissions to Middlemore Hospital • Length of Stay in Middlemore • Readmission rate Process Measures • Numbers of patients identified with COPD in primary care. • Numbers of patients receiving all or parts of early diagnosis primary care bundle. • Numbers of patients offered, attending and completing community based pulmonary. • Numbers of patients receiving discharge care bundle. • COPD patients by localities Highlights and Lowlights - Highlights - Working across primary and secondary care. - Forming, what has become the COPD Team to work on the secondary care bundle. - Having the opportunity to review best practices, adapting and testing them for our patients and community. - Partnering with Auckland & Waitemata DHB’s for the COPD primary care pathway. - Sharing ideas and learning’s with Northland DHB and Canterbury - Lowlights - The challenges of testing when there are no patients. - Finding a meeting time that everybody can attend.