Mixed Connective Tissue Disease Dan Mandel, MD
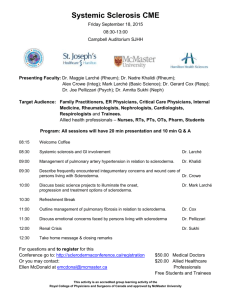
advertisement

Mixed Connective Tissue Disease Dan Mandel, MD Mixed Connective Tissue Disease • Autoimmune Disease • Features of: • • • • SLE Scleroderma Inflammatory Myositis (Polymyositis) Rheumatoid Arthritis • Serology: positive anti U1-RNP Ab • Abreviated as MCTD Terminology • Mixed Connective Tissue disease • Patient meets criteria for MCTD generally with antibody positivity (RNP Ab) • Undifferentiated Connective Tissue disease • Patient does not meet criteria for any given autoimmune disease but has features suggesting the early features of an autoimmune disease. • Overlap Syndrome • One dominant autoimmune disease with overlap featueres of another. UCTD vs Overlap vs MCTD Undifferentiated Connective Tissue Disease Polymyositis-Scleroderma Overlap Mixed Connective Tissue Disease Epidemiology of MCTD • • • • Prevalence 3-4 per 100,000 population Female to Male Ratio is 3:1 Present in all races Peak age of Onset: 15-25 Sensitivity of ANA in Rheumatology RNP Antibody – Sensitivity is 100% in Mixed Connective Tissue Disease Specific Antibodies in Rheumatology Immunology of MCTD • Extractable Nuclear antigens: • Ribonucleoproteins extractable from nucleus • SSA, SSB, smith, RNP, Jo-1, Scl-70, others • U1-RNP Antibody – Antigen: complex of series of small ribonucleoproteins containing (U1-snRNP) • 3 polypeptides (70 kd, A, C) • Linked to U1 RNA Immunology of MCTD U1-snRNP usmle287.wordpress.com U1 RNA http://en.wikipedia.org/wiki/U1_spliceosomal_RNA Gene Splicing www.biology.arizona.edu genome.wellcome.ac.uk 70KD protein is dominant antigen U1RNA is another antigen Anti-RNP Ab • Generally the IgG anti-U1 RNP Ab is checked • IgG form is generally more associated with MCTD, while IgM form may often occur in Lupus. • When found in isolation suggests MCTD Immunology of MCTD Immunogenicity Innate Adaptive Immunology of MCTD Elevated IL-1 and IL-6 production MCTD as separate entity Clinical Features of MCTD • Early Features • Arthritis – can be erosive or non-erosive • Raynaud’s • Puffy Hands/sausage digits • Later features • Can develop skin thickening typical of Scleroderma • Can develop lupus manifestations • Can develop organ involvement: lungs, kidneys, muscle. Raynauds in Rheumatology Exam Findings In MCTD • • • • Scleroderma Features SLE (Lupus) Features Inflammatory Myositis Features Rheumatoid Arthritis Systemic Sclerosis (Scleroderma) • Limited Scleroderma • Skin thickening is distal to elbows and knees, not involving trunk • Can involve perioral skin thickening (pursing of lips) • Less organ involvement • Seen in CREST syndrome • Isolated pulmonary hypertension can occur • Diffuse Scleroderma • Skin thickening proximal to elbows and knees, involving the trunk • More likely to have organ involvement • Pulmonary fibrosis and Renal Crisis are more common. Scleroderma Features • • • • • Calcinosis Raynaud’s Esophageal Dysmotility Sclerodactyly (skin thickening of digits) Telangiectases CREST Features ACR and Mayo Foundation Calcinosis on x-ray Gupta E., et al. Malaysian Family Physician. 2008;3(3):xx-xx ACR ACR Scleroderma Skin Manifestations Sclero.org International Scleroderma Network Kahaleh B. Rheum Dis Clin N Amer 2008:57-71 Nailfold Capillaroscopy SLE (Lupus) Features • Lupus: (MD SOAP N HAIR) • • • • • • • • • • • Malar Rash Discoid Lesions Serositis Oral Ulcers Arthritis Photosensitivity Neurologic (seizures, neuropsychiatric) Hair Loss, Hematologic (cytopenias) ANA Positivity Immunologic (ds-DNA, Smith, RNP, anti-SSA, APLA) Raynauds, Renal Malar Rash • • • • Often mildly scaly Typically involves bridge of nose Spares Nasolabial fold Generally non-pruritic but can be American College of Rheumatology Slide Collection Discoid Skin Lesions • Early: well demarkated, erythematous, indurated scaly plaques. • Late: atrophic, well demarkated scars. • Often occurs in people without Systemic Lupus Erythematosus American College of Rheumatology Slide Collection Serositis Pleural effusions www.learningradiology.com Pericarditis www.bukisa.com • Chest Pain • Acute Abdomen reference.medscape.com Peritonitis reference.medscape.com Other Features of Lupus Arthritis/Arthralgias Oral Ulcers Photosensitivity Neurologic Manifestations of Lupus • • • • Seizures (rare in MCTD) Neuropsychiatric Lupus/Psychosis (rare in MCTD) Strokes related to aniphospholipid syndrome. Trigeminal Neuropathy (occurs in MCTD but less commonly in SLE). Other Lupus Manifestations Specific Antibodies Anti-RNP Anti-ds-DNA Anti-Smith Anti-SSA Antiphospholipid Hair loss / Alopecia www.dermhairclinic.com ANA Positive en.wikipedia.org Immunologic Raynaud’s Syndrome Inflammatory Myositis Features • Symptoms • Proximal Muscle weakness » Difficulty getting out of chairs or getting up from crouching » Difficulty lifting objects overhead • Generally is painless, though may have mild pain • Generally without significant muscle tenderness • Laboratory Tests: • Elevated muscle enzymes (CK, AST>ALT, Aldolase, Myoglobin) • Normal inflammatory markers: ESR and CRP Inflammatory Myositis Exam www.clinicalrehabspecialists.com meded.ucsd.edu at.uwa.edu Inflammatory Myositis Manifestations & Workup • http://www.iomonitoring.pro/emg.htm Inflammatory Myositis Manifestations & Workup Olsen NJ, et al. Rheum Dis Clin N. Amer 1996;22(4):783-796 http://www.rayur.com/muscle-biopsy.html Inflammatory Myositis Manifestations & Workup Arq. Neuro-Psiquiatr. vol.62 no.4 São Paulo Dec. 2004 • Biopsy helps to confirm disease Classification Criteria for MCTD MCTD Manifestations and frequency Serologies in MCTD Features of Diseases Feature MCTD SLE Scleroderma Polymyositis Renal Involvment Less Common Common Renal Crisis may occur Rare Pulmonary PAH/ILD Less common PAH/ILD ILD may occur Esophageal Dysmotility Common Rare Common Uncommon, but dysphagia Antiphospholipid Syndrome Less common Common Less common Less common Cytopenias Can Occur Common Rare Rare Sclerodactyly Common Rare Common Rare Neurological Less Common, (trigeminal) More Common Rare Rare Treatment of MCTD • Arthritis • • • • Prednisone Hydroxychloroquine Methotrexate Biologics (Rituxan, Orencia, anti-TNF) – generally with erosive disease and/or RF/CCP positive. Treatment of MCTD • Raynaud’s • Nifedipine or amlodipine • Sildenafil • Nitroglycerine (not used as much – had been used as patch or ointment – cannot use with sildenafil) • Digital Ischemia – acute • • • • Hospitalization with IV prostoglandins Anticoagulation with heparin Search for hypercoagulability (Antiphospholipid Ab) Evaluation for vasculitis / arterial obstruction Treatment of MCTD • Scleroderma Skin • Often no treatment for limited disease • Methotrexate • Mycophenolate Treatment of MCTD • Inflammatory Myositis • • • • • • Prednisone Methotrexate Azathioprine Rituximab mycophenolate IVIG Treatment of MCTD • Pulmonary Involvement – Interstitial Lung Disease • • • • • Prednisone Mycophenolate Cyclophosphamide Rituximab Azathioprine maintenence – Pulmonary Hypertension • Vasodilators (Ca chanel blockers, sildenafil, prostoglandin) Treatment of MCTD • Lupus Type Manifestations – Depends on manifestations • • • • • • • • Prednisone Hydroxychloroquine Mycophenolate Azathioprine Methotrexate Belimumab (Benlysta) Rituximab IVIG Treatment of MCTD • Lupus Arthritis • Prednisone • Hydroxychloroquine • Methotrexate • Oral Ulcers • Hydroxychloroquine • Topical steroids • Raynaud’s • Vasodilators Treatment of MCTD • Malar Rash • • • • Prednisone Hydroxychloroquine Mycophenolate Azathioprine • Thrombocytopenia • • • • Prednisone IVIG Rituximab Plaquenil Treatment of MCTD • Leukocytopenia • • • • Often no treatment required Prednisone Hydroxychloroquine Mycophenolate • Antiphospholipid Syndrome • • • • • Anticoagulation IVIG Rituximab Plaquenil Avoid estrogen (avoid OCP’s with estrogen) Treatment of MCTD • Lupus Nephritis • • • • Prednisone Mycophenolate Cyclophosphamide Azathioprine • Pericarditis/Pleuritis • NSAIDs • Prednisone Prognosis in MCTD • Survival Rates • 5 yrs: 98% • 10 yrs: 96% • 15 yrs: 88% • Major causes of death • • • • Pulmonary hypertension: 9/280 patients Cardiovascular events: 7/280 TTP: 3/280 Infections 3/280 J Rheumatol. 2013 Jul;40(7):1134-42 MCTD Phenotypes Antiphospholipid Myositis/ILD RA/Scleroderma Survival of Phenotypes Myositis/ILD RA/Scleroderma Antiphospholipid Case 1 • A 47 year old female with Raynaud’s symptoms and puffy hands, hand pain,who presents with difficulty lifting objects overhead and leg weakness. • Exam • Fluctuating pallor/cyanosis of few digts of hands • Lungs are clear • No sclerodactyly, oral ulcers, malar rash, alopecia • Strength significantly reduced in proximal upper and lower extremities; normal distally; neck strenght intact. • Labs • ANA positive, RNP Ab positive, ESR 10, CRP 0.5 • CK level 5000, Aldolase elevated • Antiphospholipid Ab’s negative, C3 & C4 normal, UA normal; antiSmith/SSA/SSB/Jo-1/ds-DNA negative • What is the next step, diagnosis and treatment. Case 1 • Next steps: • Obtain MRI of weakest thigh or proximal arm • Obtain muscle biopsy • CXR baseline is normal • Diagnosis • Mixed Connective Tissue Disease with primary features of Polymyositis • Treatment • Start Prednisone • Start methotrexate or azathioprine • Course: • Over a period of months strength gradually improves and CK level declines; there is decrease in puffy hands and hand pain with treatment. Case 2 • A 60 year old female with history of Mixed Connective tissue disease with positive RNP antibody, sclerodactyly, Raynaud’s, past inflammatory myositis presents with left lower extremity DVT; lab tests are performed at the time. • Exam • Sclerodactyly to MCP joints in both hands • Lungs are clear • No oral ulcers, malar rash, alopecia • Strength intact. • Labs • ANA positive, RNP Ab positive, ESR 30, CRP 1.0, CK normal • C3 & C4 normal, UA normal; anti-Smith/SSA/SSB/Jo-1 negative • Anticardiolipin Ab 80, Lupus anticoagulant positive, B2 GP Ab negative. • What is the treatment, diagnosis, possible complication. Case 2 • Treatment/Next Step • Anticoagulation with Lovenox bridge to coumadin • Repeat antiphospholipid antibodies in 12 weeks; if still present, patient will require indefinite anticoagulation. • Diagnosis • Mixed Connective Tissue disease with scleroderma and myositis components with secondary antiphospholipid syndrome. • Potential Complication • Pulmonary hypertension with antiphospholipid antibodies Case 3 • A 22 year old female previously healthy develops Raynauds, malar rash, and oral ulcers in the past 3 months. She has had fatigue and joint pain without swelling involving the hands. She denies dry eyes or dry mouth. LMP 1 week ago. • Exam • Malar rash sparing nasolabial fold and oral ulcers noted, mild fluctuating cyanosis of several digits noted during visit, puffy hands. • Lungs are clear, oral mucosa moist. • No sclerodactyly or alopecia noted. • Strength intact. • Labs • ANA positive, RNP Ab positive, anti-SSA positive ESR 90, CRP 1.2, CK normal, low C3 and C4. • UA normal; anti-Smith/SSB/Jo-1/ds-DNA negative • Antiphospholipid antibodies negative, urine pregnancy test neg. • What is the diagnosis, treatment, important counseling information. Case 3 • Diagnosis: • Mixed Connective Tissue Disease with primary features of Lupus (SLE) • Treatment • Start Prednisone • Start hydroxychloroquine (Plaquenil) • May need to consider Azathioprine or mycophenolate if steroid sparing agent is needed to decrease steroids. • Counseling information: • Due to lupus and positive she would need high risk OB when she would like to become pregnant. • With positive anti-SSA Ab there is 1-3% risk of neonatal lupus with heart block but this can be monitored and potentially treated. • Would be best to wait until disease is better to control to plan for pregnancy References • Up to Date • Medscape • Ortega-Hernandez OD, et al; Best Practice & Research Clinical Rheumatology 26 (2012) 61–72 • Hoffman RW; Clinical Immunology 2008 (128); 8-17 • Cappelli S, et al; j.semarthrit.2011.07.010 • Szodoray P, et al; Lupus 2012 (21); 1412-1422 • Keith MP; et al; Autoimmunity Reviews 6 (2007) 232–236 • Faye N; et al; Clin Chest Med 31 (2010) 433–449 • Schur PH; The Rheumatologist, February 2009 • Hajas A; J Rheum 2013 (40; 7) 1134-1142 • Prete M, et al; Autoimmunity Reviews xxx (2014) xxx–xxx