prescription and response to pancreatic enzyme therapy in
advertisement

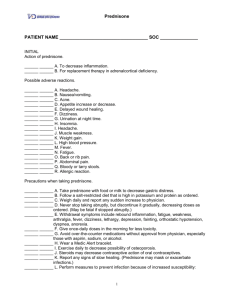
Comparable efficacy of low and high dose induction corticosteroid treatment in autoimmune pancreatitis J. Buijs¹, M.J. van Heerde¹, B.E. Hansen¹,², K. Biermann3, F.P. Vleggaar4, M.A. Brink5, E.J. Kuipers¹,6, M.J. Bruno¹, H.R. van Buuren¹ ¹ Department of Gastroenterology and Hepatology, Erasmus University Medical Center, Rotterdam, the Netherlands ² Department of Public Health, Erasmus University Medical Center, Rotterdam, the Netherlands 3 Department of Pathology, Erasmus University Medical Center, Rotterdam, the Netherlands 4 Department of Gastroenterology and Hepatology, University Medical Center Utrecht, the Netherlands 5 Department of Gastroenterology, Meander Medical Center, Amersfoort, the Netherlands 6 Department of Internal Medicine, Erasmus University Medical Center, Rotterdam, the Netherlands Autoimmune pancreatitis (AIP) is a distinct type of chronic pancreatitis highly responsive to corticosteroids. The usually recommended dosage of prednisone for remission induction is 0.6 mg/kg/day, resulting in daily starting doses of 30 – 60 mg. This recommended dosage is largely based on empirical data and lacks scientific base. Potentially, high dose corticosteroid treatment is associated with significant side effects, particularly in a population characterised by relative advanced age, diabetes and obstructive jaundice at presentation. The rationale for high dose treatment could also be questioned considering the well-established sensitivity for corticosteroids in AIP patients. We therefore compared the efficacy of treatment and the incidence of worsening glucose tolerance in AIP patients treated with different doses of steroid induction therapy. A retrospective survey was conducted of patients diagnosed with AIP between May 1992 and August 2011. Clinical, laboratory and image findings were assessed before treatment and at 1, 3 and 6 months after starting treatment. Differences between groups treated with different initial doses of prednisone were compared using linear and logistic regression analysis. A total of 37 patients (33 males; median age 65 years) were included. The most frequent presenting symptoms included jaundice, pancreatic insufficiency, weight loss and (mild) abdominal pain. Four patients were treated with an initial dose of prednisone of 10 mg/d, 2 patients with 15 mg/d, 6 patients with 20 mg/d, 11 patients with 30 mg/d, 12 patients with 40 mg/d and 2 patients with 60 mg/d. With respect to the baseline characteristics including gender, age, presenting symptoms, laboratory and imaging results, there was no significant difference in administered dose of prednisone. During a clinical follow-up period of 6 months, 37/38 (97%) patients achieved clinical response. Symptomatic response after 1, 3 and 6 months of treatment was not associated with doses of prednisone. Treatment response according to imaging studies and laboratory parameters was also comparable. There was no significant difference in worsening of glucose tolerance. (Table 1) Conclusions: Symptomatic, radiological and biochemical improvement was comparable for AIP patients treated with variable induction doses of prednisone. Based on these retrospective data it may be questioned whether high dose prednisone therapy is truly indicated in patients presenting with AIP. 2483/2900 characters (including spaces)