Clinical Decision Support Systems
advertisement

Computational Intelligence in
Biomedical and Health Care Informatics
HCA 590 (Topics in Health Sciences)
Rohit Kate
Clinical Decision Support Systems
1
Reading
• Chapter 20, Text 3
2
Clinical Decision Support
• Medical practice is essentially medical decisionmaking
Types of medical decisions:
• Diagnosis: Analyze available data to determine
explanation for a patient’s symptoms
• Diagnostic Process: What tests, procedures etc.
to perform for diagnosis taking into account the
financial costs and value of the results
• Management: Treat the patient or allow the
process on its own? What treatment to be used?
Role of Computers in
Clinical Decision Support
• A clinical decision support system is any computer
program designed to help healthcare
professionals to make clinical decisions
• Programs must have
– Access to accurate data
– Extensive clinical background knowledge
– Intelligent problem-solving capabilities which takes
into account cost-benefit trade-offs and efficiency
Types of Computer Tools
• Tools for Information Management: Information
retrieval systems that can store and retrieve clinical
knowledge
– Do not help in applying that information to a task
– Interpretation is left to the clinician
• Tools for Focusing Attention: Flag abnormal values,
alert about drug interactions, remind the user of
overlooked diagnoses
• Tools for Providing Patient-Specific
Recommendations: Provide custom-tailored advice
based on patient-specific data
– We will focus on this here
Historical Perspectives: Leeds
Abdominal Pain System
• In late 1960s F. T. deDombal and his associates at
University of Leeds developed computer-based
decision aids using Bayesian probability theory
• Their system used Bayes’ theorem to calculate
probability of seven possible explanations for
acute abdominal pain
– Conditional independence assumption of the findings
of various diagnoses
– Mutual exclusivity of the seven diagnoses
Leeds Abdominal Pain System
• Evaluation (1972)
– Using the clinical and laboratory findings for 304 patients
who came to emergency room with abdominal pain onset
• Clinicians’ diagnoses were correct 65-80 % of 304 cases
• The program’s diagnoses were correct 91.8 % of 304 cases
• The system achieved widespread use in emergency
department
• Although never achieved the same degree of accuracy
on other settings
• Perhaps because of different probabilistic relationships
between findings and diagnoses in different patient
populations
Historical Perspectives: MYCIN
• MYCIN program (mid-late 1970s) concentrated
on management of patients who have
infections
• The developers doubted statistical methods
for the purpose and so used rule-based
methods
• Knowledge of infectious diseases was
represented as production rules
• A production rule is a conditional statement
that relates observations to inferences
A MYCIN Production Rule
• Rule507 (English translation):
If:
•
•
•
•
•
The infection that requires therapy is meningitis
Organisms were not seen on the stain of the culture
The type of infection is bacterial
The patient does not have a head injury defect
The age of the patient is between 15-55 years
Then:
• The organisms that might be causing the infections are
diplococcus-pneumoniae and neisseria-meningitidis
MYCIN
• MYCIN determined which rules to use and
how to chain them to make decisions
• Rules were in machine-readable format,
English translation could be displayed
• Could display its explanations to the user
• System developers could modify the
program’s knowledge structure by removing,
adding or altering rules
Evaluation of MYCIN
• Evaluated for blood-borne bacterial infections
and meningitis
• MYCIN gave advice that compared favorably
with that offered by experts
• It was never deployed clinically, but paved way
for research and development in 1980s
• Helped in the surge of rule-based approaches
in AI in the early 1980s
Historical Perspectives: HELP
• HELP (Health Evaluation through Logical Processing)
• An integrated hospital system developed at LDS Hospital in
Salt Lake City, from 1970s
• HELP has ability to generate alerts when abnormalities in
the patient record are noted
• Adds to a conventional medical-record system a monitoring
program
• Created and adopted a standard formalism for encoding
decision rules known as Arden syntax
• Arden syntax is a programming language that provides a
canonical means for writing rules that relate patient
situations to appropriate actions to be taken
• Each decision rule is called medical logic module (MLM)
A Medical Logic Module in
Arden Syntax
Penicillin_order :=event
{medication_order where class=penicillin};
/* find allergies */
Penicillin_allergy :=
read last {allergy
where agent_class = penicillin};
;;
evoke: penicillin_order;;
logic:
If exist (penicillin_allergy) then conclude true;
endif;
;;
action:
write “Caution, the patient has the following allergy to penicillin
documented:”
|| penicillin_allergy
HELP System
• Whenever new data for a patient becomes
available, the HELP system checks whether the
data matches the criteria for invoking an MLM
• The logic of MLMs has been developed by
clinical experts
• The output of MLMS include: alerts regarding
drug reactions, interpretation of lab tests,
calculations of the likelihood of diseases
Evaluation of HELP
• Several studies in the 1980s demonstrated the
beneficial effect of HELP at LDS Hospital
• Demonstrated how integration of decision
support with other system functions can increase
its acceptance and use
• Hospital systems have evolved towards more
distributed architectures (several computers
involved), HELP served as a model for decision
support over an integrated data monitoring
architecture
Lessons Learned from Early
Decision Support Systems
• Clinical value of Bayesian diagnostic system
demonstrated by Leeds abdominal pain system,
subsequently more Bayesian systems were built,
e.g. Pathfinder system for lymph-node pathology
• MYCIN and HELP demonstrated the use of
knowledge representation in encoding medical
knowledge
• Most early decision-support systems were rarely
used in real practice and were viewed with
skepticism but the attitudes are now changing
Changing Attitudes Towards
Decision Support Systems
• Emergence of personal workstations and WWW along
with easy-to-use interfaces
• Recognition by the developers that their system must
meet work practices of those who will use it
• Growing amount of medical information
• Fiscal pressure to practice cost-effective evidence-based
medicine
All this is leading to increasing acceptance of the ideas of
computer-based decision tools
See:
–
–
Several clinical decision systems in practice:
http://www.openclinical.org/aisinpracticeDSS.html
Other AI clinical systems in practice:
http://www.openclinical.org/aisinpractice.html (right side menu)
Illustrative Example: Internist-1
and QMR Project
• Internist-1 was a large diagnostic program
developed at the University of Pittsburgh in the
1970s
• Contained knowledge of almost 600 diseases and
4500 findings (signs, symptoms, patient
characteristics)
• Decided against estimating conditional
probabilities because some diseases are rare and
not so well described in literature, instead used
an ad hoc scoring scheme to relate findings and
diseases
Internist-1
• One senior physician (50+ years of experience)
and other physicians, medical students worked
together considering each disease
• Through literature review and case discussions
determined a list of pertinent findings associated
with each disease and scored the following
– Frequency weight (1-5): How frequently the finding
occurs with the disease
– Evoking strength (0-5): How likely is the finding
because of the disease
– Import number (1-5) with each finding: The need to
explain the finding
Internist-1
• The physician-user would enter an initial set of
findings, and then the program would determine
an initial differential diagnosis
• The program would select appropriate questions
to ask
• Would recommend lab tests and diagnostic
procedures after doing cost and benefits analysis
• Could diagnose multiple diseases and did not
make mutual exclusivity assumption as in
Bayesian programs
Internist-1 Evaluation and QMR
• 19 patients had a total of 43 diagnoses
– Internist-1 identified 25
– Physicians identified 28
– Experts who presented the case identified 35
• In the 1980s, the program was adapted to run on personal
computers as QMR (Quick Medical Reference)
• QMR also served as:
– Electronic textbook: Listing patient characteristics for a disease
etc.
– Medical spreadsheet: Obtain suggestions about coexisting
diseases
– Developers argue that electronic reference is more important
than the consultation program
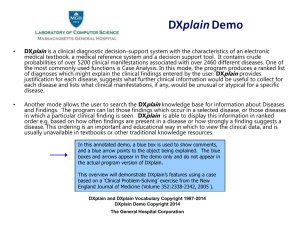
Illustrative Example: DXplain System
• DXplain system developed at Laboratory of Computer Science
at the Massachusetts General Hospital in the late 1980s
http://lcs.mgh.harvard.edu/projects/dxplain.html
• Given a set of clinical findings (signs, symptoms, laboratory
data), DXplain produces a ranked list of diagnoses that might
explain (or be associated with) the clinical manifestations
• DXplain provides
– justification for why each of these diseases might be
considered
– suggests what further clinical information would be useful
to collect for each disease
– lists what clinical manifestations, if any, would be unusual
or atypical for each of the specific diseases.
• Not intended to be used as a substitute for human clinician
Dxplain
• Has a large database of crude probabilities of
over 4500 findings associated with 2000 different
diseases
• Adopts a modified form of Bayesian reasoning
• Used by a number of hospitals and medical
schools, mostly for educational purposes but also
for clinical consultation
• The most extensively used decision-support tool
today
• Could be used as electronic medical textbook and
a medical reference system
Illustrative Example: EON
Architecture
• EON constitutes a set of software components that must be
embedded within some clinical information system
• The components in EON are designed such that they can be
mixed and matched to create different decision-support
functionalities
• Plugging in a knowledge-base of AIDS and HIV related
disease, it becomes a decision-support system for AIDS
(THERAPY-HELPER)
• Plugging in a knowledge-base of breast cancer it becomes a
corresponding decision-support system
• The knowledge-bases are provided as an ontology, typically
developed using a tool like Protege
Illustrative Example: GIDEON
• GIDEON (http://www.gideononline.com/)
– A global infectious disease knowledge management tool
– Easy to use, interactive and comprehensive web based tool
– Support for the diagnosis and treatment of infectious
diseases, knowledge base is updated weekly about
diseases and their trends
– Hundreds of customers from around the world, including
educational institutions, hospitals, public health
departments and military organizations, use it as their
diagnosis and reference tool for Infectious Diseases,
Microbiology and Occupational Toxicology
– Requires monthly or yearly subscriptions
AI in Medicine: Example Systems
From: http://www.gideononline.com/
Legal Issues
• Formal legal precedents for dealing with clinical
decision-support systems are lacking at present
• Should the systems be viewed under negligence
law or product liability law
• It is unrealistic to expect systems to perform
flawless, even physicians don’t perform flawless
• May be potential liability borne by physicians
who could have accessed such a program, and
who chose not to do so, and who made an
incorrect decision when the system would have
suggested the correct one
Legal Issues
• Several guidelines have been suggested for assigning legal
liability to builders of knowledge-based medical decisionsupport systems or to the physicians using them
• Validation of system before their release is challenging and
it is difficult to determine acceptable levels
• Current policy of the Food and Drug Administration (FDA) in
the United States indicates that such tools will not be
subject to federal regulation if a trained practitioner is
assessing the program’s advice and making the final
determination of care
• However, programs that make decisions directly controlling
the patient’s treatment (e.g. closed-loop systems that
administer insulin or that adjust intravenous infusion rates
or respirator settings) are viewed as medical devices
subject to FDA regulation
Future of Clinical DecisionSupport
• Concerns about cost and quality of patient care
globally have altered the practice of medicine
• Clinical practice guidelines based on empirical medical
evidence are now ubiquitous
• Decision-support systems will play a central role
• Internet has greatly simplified information access
• New pressures to learn best practices coupled with the
ubiquity of information technology, have greatly
encouraged the use of computer-based decision aids in
health-professional schools around the world and this
trend is likely to continue
•
Future of Clinical DecisionSupport
Combining different reasoning methods to meet the
specific requirements of increasingly complex decisionmaking tasks
–
–
–
–
Bayesian reasoners for performing probabilistic classification
Rule-based methods for encoding human knowledge
Machine learning methods to learn from data
Mathematical models for solving problems that can be best
understood analytically in terms of systems of equations
– A suitable combination of the above as appropriate for the need
• Heightened understanding of organizational behavior and
of clinical workflow will stimulate a new generation of
clinical information systems that will integrate smoothly
into the practices of healthcare workers of all kinds
• The very concept of a decision-support system itself will
fade away as they blend into the infrastructure of
healthcare delivery
AI in Medicine: Issues
• Although there has been a remarkable progress
in AI in Medicine but adoption of these methods
have been slow, mostly because of political, fiscal
and cultural reasons
– If a computer makes a wrong diagnosis leading to bad
consequences, who should be held legally
responsible?
– Many learning methods need a lot of data to learn
from, will that compromise medical data
confidentiality?
– All healthcare workers may not be computer savvy
– How much will doctors trust computers?
AI in Medicine: Issues
• AI applications are most suited in medicine in the
form of:
– Supporting tools instead of a stand-alone systems, for
example, in suggesting possible diagnoses and their
probabilities
– Covering human mental shortcomings/lapses
• Forgetfulness: reminders of certain tests or medications
• Detect possible errors
– Searching and mining huge amounts of data which is
not humanly possible and present results to humans
Computational Intelligence
• In this course we covered the following AI topics along with
their medical applications
–
–
–
–
Probability and Probabilistic Reasoning
Machine Learning
Data Mining
Knowledge Representation
• Description Logic
• Ontologies
– Natural Language Processing
• Some AI topics we did not cover
– Computer Vision: (processing images, e.g. in radiology)
– Robotics
– Planning (planning and scheduling in a hospital environment)
AI in Medicine: Some Resources
• Artificial Intelligence in Medicine
– Journal published by Elsevier, accessible online through library’s website
• AIME: A European biannual conference of AI in Medicine
• Other medical informatics journals and conferences also
routinely include AI in medicine topics
• OpenClinical.org
– An online resource for knowledge management systems in healthcare
includes AI in Medicine (http://www.openclinical.org/aiinmedicine.html)
• Artificial Intelligence in Medicine, edited by Peter Szolovits
– An old outdated book but still interesting, entirely available online
• http://groups.csail.mit.edu/medg/ftp/psz/AIM82/