Ant-Infective Drugs - bbrushpharmacology
advertisement

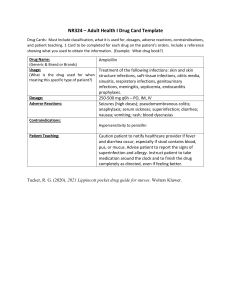
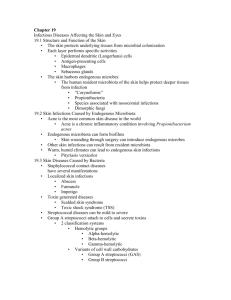
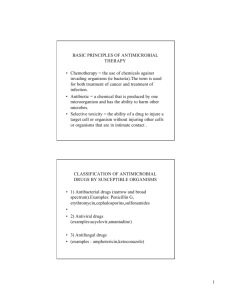
Ant-Infective Drugs • Antibacterials • Sulfa Drugs • Urinary • Anti-tuberculosis • Antifungals • Antivirals Antibacterial Drugs (Antibiotics & Antimicrobials) I. Increased Susceptibility to Infection A. Age B. Exposure C. Barrier Disruption D. Immune Defenses E. Circulation F. Nutrition II. Identification of Organisms A. Microscope B. Gram Stain C. Culture D. Sensitivity III. Selection of Agent A. Location B. Organ Function (liver, kidney) C. Age (very young vs elderly) D. Pregnancy / Lactation E. Resistance (MRSA, VRE) F. Know allergy IV. Classification A. Action 1. Bacteriocidal 2. Bacteriostatic B. Spectrum 1. Broad 2. Narrow C. Antibiotic vs Antimicrobial V. Actions VI. Uses A. Primary Infection B. Secondary Infection C. Pre-op D. Prophylaxis E. Virus - no! F. Nosocomial infections VII. Adverse Reactions A. Hypersensitivity/ Anaphylaxis B. Cross-Sensitivity C. Organ Toxicity - direct 1. Nephrotoxicity 2. Hepatotoxicity 3. Ototoxicity D. Hematological – blood dyscrasias E. Superinfection (indirect) F. Pain - phlebitis G. GI Distress H. Neurotonic VII. Antibacterial Agents A. Penicillins B. Cephalosporins C. Tetracyclines D. Aminoglycosides E. Sulfonamides F. Miscellaneous: 1. Macrolides – erythromycin 2. Quinolones - Cipro X. Aminoglycosides (gentamycin) A. Action: gram neg & resistant B. Use 1. Urinary infections - resist 2. Pre-op for intestinal OR C. Adverse Effects: N/V/D 1. Nephrotoxicity - BUN 2. Ototoxicity - tinnitis D. Interactions: general anesthesia (Neuromuscular blocking)-flag E. Peak & Trough levels (1hr/30min) IX. Cephalosporins – semi-synth A. Use - penicillin resistance B. Generations – broad spectrum 1. First - Keflin 2. Second - Ceclor 3. Third – Claforan (&4th) C. Cross sensitivity to penicillin D. Adverse reactions 1. Nephrotonic, rashes 2. GI Distress – food (NVD) 3. Injection pain - phlebitis XIV. Macrolide -Erythromycin (E-mycin) A. Action - bacteriostatic B. Uses: oral therapy for penicillin substitute (least toxic) 1. Respiratory infections 2. Soft tissue (gums) infections 3. Mycoplasms, chlamydia (STD) C. S/E: 1. N/V/D 2. Skin rash, superinfection D. Helicbacoter pylori E. Dangerous interactions – ie,Diflucan VIII.Penicillins – from fungus (treat Streph, Staph& Pseudo – resp, intestinal infections, helicobacter pylori) A. Overuse Penicillin B. Natural vs synthetic C. Routes: oral, IM, IVs D. Units, grams, mgs E. S/E: GI (NVD), allergy, superinf F. Example: Amoxicillin G. Inhibits estrogen – BCP/avoid alcohol XVII. Quinolones - Ciprofloxacin: Cipro A. Resistance by son Pseudomonas B. Use:UTI, Resp, GI C. S/E: some serous 1. N/V/D, rash 2. Photosensitivity (toxic) 3. CNS: H/A, dizzy, tremor-caffeine 4. Crystalluria – drink fluids! 5. Collitis – in elderly 6. Cartilage damage in children 7. Tendon damage – no strenuous exercise D. Interactions: Many drugs! XI. Tetracyclines (tetracycline) – broad spec A. Uses: (incr. resistance) uncommon 1. Alternative to penicillin 2. Richettsiae, Lyme, chr bronchitis B. Adverse effects: 1. N/V/D 2. Superinfection 3. Photosensitivity, rash 4. Discolored teeth, retarded bone C. Contraindications: binds to calcium & iron - not w/ food D. Pregnancy, under 8 yrs of age E. Outdated - nephrotoxic XV. Chloramphenicol: A. Use: serious life-threatening infections (typhoid) & topical ocular infections (toxic!) B. S/E &Adverse reactions: 1. Fatal blood dyscrasias or bone marrow depression 2. N/V/D 3. Superinfections C. Contraindic: Infants under 2 mos (Immature livers) XVI. Miscellaneous: (Toxic) A. Vancomycin - (MRSA) various 1. organ toxicities (oto, nephro) 2. IV - necrosis B. Flagyl - antibacterial & antiprotozoan (Trichomonas) – very toxic 1. neurological 2. Avoid alcohol – disulfiram rx C. Cleocin (clindomycin)1. Colitis (life treatening) – d/c if N/V/D Antivirals A. Natural immunity or vaccination B. Many viruses do not produce immunity & vaccines not available C. Viral infections 1. Herpes simplex I & II 2. Herpes zoster (shingles), chicken pox 3. Flu, cold 4. AIDS, hepatitis D. Drugs: 1. Zovirax - cutaneous & genital Herpes, herpes zoster (acyclovir) 2. Zidovudine (AZT, Retrovir) AIDS & CMV 3. Symmetrel (amantadine) – Flu 4. Tamiflu - inhalation E. Action - prohibits viral attachment or protein synthesis F. S/E: N/V, lethargy, fatigue, H/A XII. Sulfonamides (precursor to antibiotics) A. Use: limited 1. Non-obstr. UTI’s 2. Burns - topical B. Action - bacteriostatic C. Med’s: Bactrim, Septra (comb.), Silvadene (topical) D. S/E: N/V/D, crystalluria (water), allergy, photosensitivity, blood dyscrasias, yellow urine, hepatotoxic, hypersensitivity E. Steven-Johnson syndrome- rash F. Interactions: Coumadin, hypoglycemics XVI. Macrodantin (Urinary Anti-infective) A. Use: Chronic UTI’s B. Not sulfonamide or antibiotic C. Action: does not achieve significant elevation of blood levels to be effective for systemic infections. Interfers with bacterial multip in the urine. D. S/E: N/V/D, anorexia, neuritis respir.allergy (wheezing), dark urine Antifungals A. Plant-like: yeasts or molds B. Systemic mycotic Infections 1. Serious 2. Immunosuppressed C. Dermatophytic - hair, nails, skin (athlete’s foot, ring worm) D. Candida albicans - superinfection E. Meds: 1. Fungizone (amphotericin B) systemic infections 2. Griseofulvin - hair, skin, nails 3. Mycostatin (nystatin) candida 4. Diflucan – one dose med (fluconazole) F. Action: usually fungicidal G. Adverse Effects: 1. N/V/D 2. H/A & dry mouth H. Hospitalized for IV systemic trmt (serious side effects) XIII. Ioniazid: (INH - DOT therapy) A. Use - tuberculosis (mycobacterium) 1. Asymtomatic: 6-12 months 2. Active: 2-3 agents (6-9 mos+) B. Other first line agents: 1. Rifampin 2. Ethanbutol C. S/E or Adverse Rx: (ioniazid) 1. hepatotoxicity 2. N/V - give with food 3. Neuro - numbness, tingling (given with B6)