Allergy - Stoller Design Group
advertisement
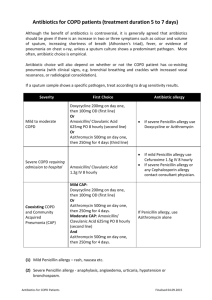
Module 3 (of 3): Allergy Review * Allergy to β-lactam Antibiotics By Keith Teelucksingh, PharmD Infectious Disease Pharmacist, Kaiser Permanente Vallejo With contributions from Linh Van, PharmD Infectious Disease Pharmacist, Kaiser Permanente Oakland See Notes Goal The goal of this presentation is to provide pharmacists with up-to-date information regarding penicillin allergy and the cross reactivity with related antibiotics. Objectives After completing this module, the participant will be able to: 1. Describe the different types of allergy (per Gell Coombs classification) as they relate to penicillin and the β-lactam-related antibiotics. 2. Be able to identify clinical situations where it is safe or unsafe to use β-lactam-related antibiotics given a patient’s allergy history. Allergy to the β-lactam antibiotics There are several classification schemes. They can be applied to other drug classes but are best characterized for the β-lactam antibiotics: Gell and Coombs Based on immunopathologic reactions (all of which have been seen w/β-lactam antibiotics). Levine Reactions specific to penicillin (PCN) according to time of onset. Gell Coombs Classification Type Type Type Type I: IgE mediation II: Antibody mediation III: Immune complex mediation IV: Delayed hypersensitivity reaction Type I: IgE mediation Serious and life threatening Can include erythema, pruritis, urticaria (hives), angioedema, bronchospasm, hypotension, arrhythmias. Mechanism Interaction of β-lactam antigens with preformed β-lactam specific IgE bound to mast cells causes release of histamine, proteases, prostaglandins, leukotrienes. Type I Time course (cont’d) Usually starts <15 min after drug administration, can also occur >1 hour after but less common. Pearl: If patient has type I hypersensitivity to PCN, unless patient has tolerated before, probably judicious to avoid cephalosporins. If unable to get specific history as to what type of rash occurred and in what timeframe, err on the side of caution. If PCN use is absolutely indicated, consult allergy for skin testing (e.g., PCN for neurosyphilis). Type II: Antibody Mediation Reactions Hemolysis, thrombocytopenia, neutropenia, interstitial nephritis Mechanism Result when β-lactam specific cytotoxic antibodies (usually IgG or IgM) become attached to circulating blood cells or renal interstitial cells that have βlactam antigens bound to their cell surface. The antibody-antigen complex can activate complement system (resulting in cell lysis), neutrophil or macrophage attachment (leading to cell injury). Type II Time course (cont’d) Usually longer term, > 7 days Pearl Long term, high-dose β-lactam treatment predisposes to this reaction (nafcillin for endocarditis, high-dose Zosyn® for Pseudomonal infection). Type III: Immune Complex Mediation Serum-sickness like reaction Mechanism β-lactam specific IgG or IgM antibodies may form circulating complexes with β-lactam antigens. These complexes can fix complement and lodge in tissue sites, possibly causing serum sickness/drug fever. Type III (cont’d) Time course: 6–21 days after exposure Pearl Best example is classic serum-sickness like reaction seen with cefaclor. Signs/symptoms: fever, arthralgia, lymphadenopathy, skin eruption Type IV: Delayed Hypersensitivity Delayed hypersensitivity reaction Contact dermatitis, delayed non-urticarial rashes. Mechanism T-cell mediated release of cytokines causing tissue inflammation and injury. Type IV (cont’d) Time course: not well defined Pearl/example Penicillin was available topically in the past, but high rate of dermatitis led to its discontinuation as a marketed product. Idiopathic Reactions Not included in Gell Coombs classification since pathogenesis is not well defined. Examples Maculopapular reactions (rash, etc.) Occurs in 2 percent to 3 percent of penicillin courses, usually late in treatment. Eosinophilia Stevens-Johnson syndrome Exfoliative dermatitis Choosing an Antibiotic Always note the REACTION to a given drug Nausea, vomiting, GI upset are NOT allergic reactions. Rash reactions: Need to either clarify type of rash and onset or err on side of caution and use alternative agents with low chance of cross reactivity. Cross-Reactivity If patient is allergic to: 1. Penicillin Can this be used? Penicillin-class drug (amoxicillin, ampicillin, etc.) 2. Penicillin Cephalosporin 3. Cephalosporin Penicillin 4. Penicillin Carbapenem Penicillin – Penicillin Class If patient has IgE mediated reaction to penicillin, likely to have similar reaction to ampicillin, amoxicillin, dicloxacillin and piperacillin. Patients with allergy to penicillin may be prone to allergic reactions to drugs in general. Aztreonam seems to be safe to use even in patients with Type I reactions. Use caution in patients with ceftazidime allergy, since these drugs have the same side chain. Reactions still can occur but tend to be very rare. Penicillin – Cephalosporin Incidence may have been higher with earlier preparations of cephalosporins . In general, patients with documented Type I reactions to penicillin should not be challenged with a cephalosporin unless there is documentation that patient has tolerated cephalosporins in the past. No good answer at this time. Cephalosporin - Penicillin Allergic reactions to cephalosporins in the general population tend to be rare. Chance of cross-reactivity between patients with cephalosporin allergy being exposed to penicillin may be higher (50 percent) with first-generation cephalosporins than that with second or third generation (~10 percent). For example, if a patient is allergic to cefazolin and exposed to a penicillin-class drug, s/he may be more likely to have an allergic reaction. If the patient is allergic to either cefuroxime or ceftriaxone, s/he may be less likely to have an allergic reaction to a penicillinclass drug. Penicillin – Carbapenem Incidence was thought to be close to 50 percent. Emerging data suggests that carbapenems may be safe to use in patients with Type I penicillin allergy. Some data to suggest that patients with type IV reactions to penicillins will have a ~5 percent chance of cross-reaction with carbapenems (imipenem). References Chen, S. Serum sickness. http://emedicine.com Weiss, M., Adkinson, N. Chapter 24: β-lactam Allergy. Mandell, Bennett & Dolin. Principles and Practice of Infectious Disease. 7th ed. 2009. Robinson, et al. Practical aspects of choosing an antibiotic for patients with a reported allergy to an antibiotic. Clin Infect Dis. 2002 Jul 1;35(1):26-31. Patriarca, et al. Tolerability of aztreonam in patients with IgE-mediated hypersensitivity to beta-lactams. Int J Immunopathol Pharmacol. 2008 Apr-Jun;21(2):375-9. Schiavino, et al.Cross-reactivity and tolerability of imipenem in patients with delayedtype, cell-mediated hypersensitivity to beta-lactams. Allergy 2009 Apr 14. Romano, et al. Brief communication: tolerability of meropenem in patients with IgEmediated hypersensitivity to penicillin. Ann Intern Med. 2007 Feb 20;146(4):266-9 Prescott, et al. Incidence of carbapenem-associated allergic-type reactions among patients with versus patients without a reported penicillin allergy. Clin Infect Dis. 2004 Apr 15;38(8):1102-7 Acknowledgments Thank you to the following individuals for their support of and/or assistance with this program: Dan Dong, Pharm D, Area Pharmacy Director Kaiser Permanente East Bay Service Area Kathleen Hiroshima, Pharm D, Drug Information Services Kaiser Permanente California Regions Matangi Venkateswaran, Pharm D, Inpatient Quality-Clinical Supervisor, Kaiser Permanente Central Valley Service Area Sam S Lee, Pharm D, Inpatient Pharmacy Supervisor Kaiser Permanente Santa Rosa Conclusion * This concludes Module 3 of the Review of Basic Principles and Selected Antimicrobials. Upon completion of Modules 1, 2 and 3, you may proceed to the post-test and evaluation. Thank you for participating in this continuing education program. See Notes