Diabetes & Osteoporosis
advertisement
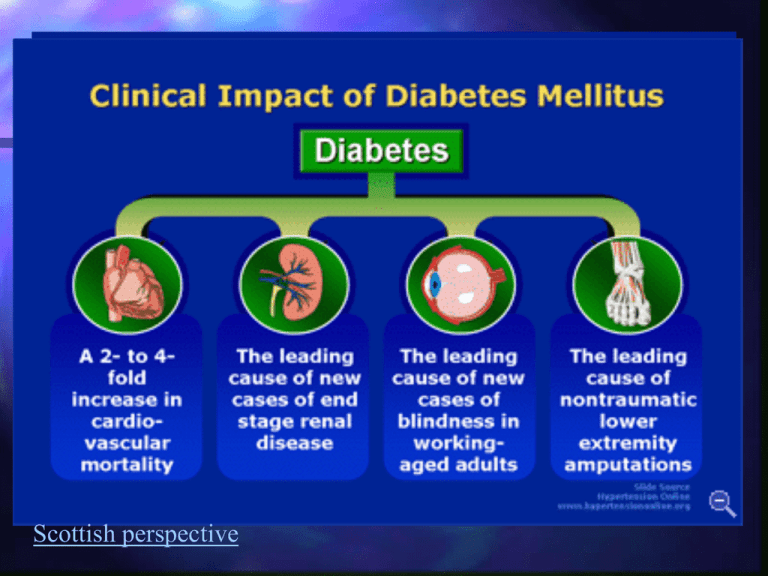
Diabetes Mellitus Failure to control blood glucose Long term health complications Atherosclerosis Stroke Neuropathy (damaged nerves) Retinopathy, glaucoma Scottish perspective Control of Blood glucose If blood glucose rises If blood glucose falls Excess is stored in muscles & liver as glycogen Deficit remediated by breaking glycogen down in liver and releasing into blood stream Two hormones: Insulin & Glucagon Control of Blood glucose Insulin: Synthesised by cells of Islet of Langerhans in pancreas Glucagon Synthesised by cells of Islet of Langerhans in pancreas Blood glucose level sensed in pancreas Regulates secretion of insulin/ glucagon directly Negative feedback system (p54) INSULIN – target cells Insulin acts on Insulin increases permeability of fat/ skeletal muscle cell membrane to glucose Liver Adipose tissues (fat) Skeletal muscle cells So stimulates glucose uptake into these tissues Liver already very permeable Insulin stimulates glycogen formation & glucose uptake INSULIN Insulin acts via an insulin receptor Diabetes occurs through two mechanisms 1 – Loss of insulin 2 – Loss of insulin receptors Diabetes in Young Adults (15-30 years) Type 2 Type 1 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90 Age of diagnosis Genetic Nurses in Diabetes treatment unusual genetic type of diabetes called maturity onset diabetes of the young 6 different genes causing this type of diabetes. genetically defined subtype present different clinical course. one subtype responds to sulphonylureas patients replace insulin treatment sometimes after being on insulin for over 30 years, finding the genetic cause of their diabetes has had a major impact on their treatment. Type 1 Diabetes – Insulin dependent Type 1- Diabetes (5-10%) Loss of insulin – destruction of pancreatic cells Early onset Weight loss, fatigue, polydypsia, polyuria, glucosuria, hyperglycaemia Ketosis (sweet breath – due to acetone) Treat with injections of insulin Glucose tolerance test A large bolus dose of glucose administered (100g glucose drink) Blood glucose monitored Rapid fall after peak (9-10mM) levels reached If diabetes clearance is very slow – in urine, peak blood glucose level higher Type 2 Diabetes – Insulin Independent 90-95% cases of diabetes Late onset (after 40yrs age) 3-7% population affected 60% SUMO wrestlers c.f. 5% Japanese population Mainly occurs in overweight individuals Insulin Resistance Symptoms Insulin resistance Normal or elevated blood insulin levels Failure of insulin to act on target tissues Deficiency in insulin receptors Can lead to cell function becoming compromised due to excessive insulin production Hyperglycaemia, polydypsia, polyuria, glucosuria Progression Elevated blood glucose associated with diabetes damages blood vessels and nerves Small blood vessel damage causes blindness, kidney failure & amputation Larger blood vessel damage can cause heart disease, high blood pressure & stroke 75% of Type 2 patients die of cardiovascular disease Exercise & NIDDM Insulin sensitivity in fit individuals is greater Insulin sensitivity decreases with age i.e. cells better able to uptake glucose from blood This decrease reduced by exercise 5-7 days after exercise insulin sensitivity starts to decline Regular, moderate, aerobic exercise is important in preventing onset of NIDDM Diseases control in 80-90% patients achieved by reducing calorie intake/ exercise Glasgow Research Osteoporosis Osteoprosis – long term progressive increase in bone porosity/ brittleness Risk of fractures (shatter) Loss of height Curvature of spine Back pain Post menopausal women 20-50% over 50s 75% over 90s Bone growth Childhood and early adolescence bones extend Late adolescence bones increase in density Peak bone density in late twenties/early thirties 1%/yr (female) decline in density thereafter 2-3%/yr decline post menopausal Male bone density declines 0.4%/ yr and only when over age 50 Extra calcium/ Vitamin D in childhood & teens produce greater bone density Margaret Thatcher – cause of osteoporosis in 20102020? Risk Factors Elderly Early menopause Amenorrhoea Genetics Low body fat Low calcium in diet Vit. D deficiency High alcohol/ caffeine/ fizzy drinks High salt Age related reduction in bone density Oestrogen promotes calcium uptake Low oestrogen Enzymes in fat produce oestrogen from circulating precursors Body raids calcium stores in bones Poor calcium absorption Promote bone loss by using calcium stores to balance pH Calcium removed along with Na in the urine Exercise & Osteoporosis – Prevention Mechanical stress increases bone strength (density) Astronauts have lowered bone density following zero gravity because no mechanical stress Weight bearing or resistance exercise will benefit women in late twenties/ early thirties (swimming will not!) Also benefits coordination reducing risk of falls Exercise & Osteoporosis – Treatment 45 min moderate exercise 3 times weekly increases calcium deposition in osteoporosis patients In conjunction with HRT Risk of Exercise in Women Excessive exercise particularly in young women can cause osteoporosis Reduction in body fat leads to reduction in oestrogen synthesis Menstruation ceases Oestrogen falls further, reducing calcium absorption Bone loss is irreversible Advice from Osteoporosis Soc. It's a good idea to avoid: Too much protein – Lots of salt – phosphoric acid gives flavour to a lot of fizzy drinks too much can cause the body to use calcium to balance levels. Drinking too much caffeine – high sodium increases calcium lost in urine. Drinking lots of fizzy drinks – Excessive protein upsets acid balance. Calcium from bones neutralises it. Eating plenty fruit and veg should keep your body's acid balance stable. high caffeine intake affects the balance of calcium in the body. Milk in coffee will counteract this, limit intake to one or two cups a day. Letting your weight drop too low – Being underweight increases the risk of broken bones when you fall. In younger women, severe weight loss may stop menstrual periods because hormone levels drop which can also increase your risk of breaking a bone









