Diabetes Mellitus
advertisement

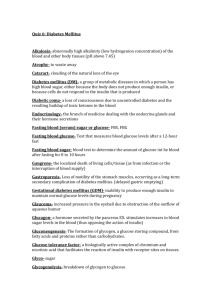
Diabetes Mellitus What is diabetes mellitus? Metabolic derangement with hyperglycemia How DM is diagnosed? Fasting plasma glucose 126 mg/dL on two occasions Random plasma glucose 200 mg/dL with symptoms Two hours glucose tolerance test with plasma glucose 200 mg/dL at 2 hour Glucose intolerance? Fasting plasma glucose >110 mg/dL and <126 mg/dL on two occasions Two hours glucose tolerance test with plasma glucose >140 mg/dL and <200mg/dL at 2 hour Other causes of hyperglycemia? Endocrine diseases: Cushing's syndrome Acromegaly Pheochromocytoma Glucagonoma Hyperthyroidism Drug-induced: Glucocorticoids Thiazides Nicotinic acid Type of diabetes? Type 1 Insulin deficiency Early age onset Acute onset Ketosis Thin Type 2 Insulin resistance Late onset Gradual, slow onset Usually non-ketotic Obese Diabetes Mellitus type 2 Epidemiology Distribution: 75-90% of diabetes mellitus Incidence: 3/1000 new cases in Caucasian populations per year (probably an underestimate) May be 2-4 times higher according to some reporting agencies Prevalence Affects 50-70/1000 people in the US A further 27/1000 have undiagnosed diabetes on the basis of fasting glucose Predisposing factors? Age: Prevalence increases with age Diagnosed at over 40, although the group with the largest and fastest increase in incidence is under age 25 Prior history of gestational diabetes Obesity Predisposing factors Race Prevalence is increased in: African-Americans Hispanic-Americans Native Americans Asian-Americans Pacific Islanders Pima Indians Socioeconomic status l Lower socioeconomic groups Predisposing factors Genetics Positive family history in 30% of cases Concordance rates of approx. 90% in identical twins One first-degree relative doubles the relative risk and two first-degree relatives increases the risk 4-fold Not associated with specific HLA genes (unlike type 1 diabetes) Polymorphisms have been identified within specific ethnic populations Polymorphisms have been identified within specific ethnic populations Symptoms? 40% are asymptomatic at diagnosis Lethargy Malaise Blurred vision Polyuria Polydipsia Frequent infections, e.g. candidiasis, balanitis, intertrigo, boils, cellulitis, urinary tract infections, vaginal yeast infections; poor wound healing Symptoms 50% already develop complicationss Eye - visual deterioration, blurred vision Neuropathy numbness/paresthesias Angina Intermittent claudication Impotence Physical findings? Obesity (BMI >26), especially centripetal obesity Eye signs - cataracts, microaneurysms, hemorrhages, hard exudates, soft exudates, new vessel formation, vitreous hemorrhage, macular degeneration Physical findings Cardiac: congestive heart failure from prior MI Foot - decreased peripheral pulses, decreased protective sensation, absent ankle-jerk reflex, ulcers Polyneuropathy, mononeuropathy (less common than polyneuropathy) Associated hypertension Associated metabolic disorders? Blood pressure ≥ 130/85 Glucose intolerance with FBS ≥ 110 mg/dL Triglyceride >150 mg/dL or HDL <40 mg/dL in males and <50 mg/dL in females Abdominal obesity with waist circumference >102 cm for males and >89 cm for female Tests? Fasting plasma glucose Hemoglobin A1c Elevated in uncontrolled diabetes, lead toxicity, iron-deficiency anemia, hypertriglyceridemia Decreased in hemolytic anemias, chronic renal failure Fasting lipid panel Bun/Cr Tests Magnesium Homocysteine – marker for cardiovascular risk Urine microalbumin and urinalysis EKG Treatments Control the hyperglycemia Management the complications Treatment options Diet Exercise Medications Stimulating insulin secretion Block hepatic gluconeogenesis Increase insulin sensitivity Decrease GI absorption of glucose Insulin Insulin secretagogues Sulonylureas First-generation – chlorpropamide, tolazamide, tolbutamide Second-generation – glyburide and glipizide Glimepiride – enhance peripheral insulin sensitivity Contraindicated in severe hepatic or renal disease Meglitinides Repaglinide, nateglinide Attenuated without exogenous glucose Contraindication in hepatic impairment Metformin Block hepatic gluconeogenesis Increase muscle sensitivity to insulin Contraindications Cr 1.5 in male and 1.4 in female CHF Contrast dye Thiazolidinediones Rosiglitazone and pioglitazone Increase peripheral sensitivity to insulin Monitor liver function tests to due to increased risk of hepatitis Arbacose Diarrhea Follow LFT periodically Contraindications Hepatic or renal impairment IBD GI obstruction Insulin Long acting for basal rate Short acting for meal May combine with oral medications Hemoglobin A1c goal? < 7% Aspirin Secondary prevention Primary prevention > age 40 with cardiovascular risk factor(s) Not less age 21 because of increased risk of Reye’s syndrome Hypertension goal? Keep blood pressure < 130/80 mmHg Cholesterol goal? LDL < 100 mg/dL Periodic exams? Annual dilated eye exam Annual monofilament test Annual urine microalbumin Annual serum creatinine Annual fasting lipid panel Hemoglobin A1c every 3 months Screening? > age 45 and every 3 years Obesity with BMI >27kg/m2 First relative with diabetes High-risk ethnic group GDM or macrosomia baby HDL 35 mg/dL and TG 250 mg/dL Disorder associated with insulin resistance such as PCO Hypoglycemia: symptoms Adrenergic symptoms: tachycardia, palpitations, tremor, anxiety, and sweating Neuroglycopenic: infaintness, feeling of hunger, headache, abnormal behavior, altered consciousness, and eventually coma Hypoglycemia: treatment Intravenous or intramuscular glucagon 1mg 20-50mL of 50% intravenous dextrose, followed by an infusion of 10-20% dextrose Neuropathy Peripheral neuropathy – Elavil or Neurontin Erectile dysfunction – Viagra Diabetic foot ulcer Control blood glucose Callus – shaving Dressing changes Osteomyelitis leading to amputation