Listeris, Legionella, and small gram
advertisement

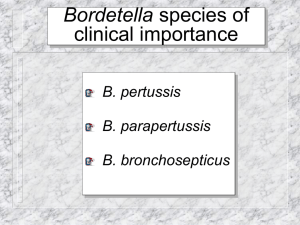
Miscellaneous Small Gram-Negative Bacilli Chapter 34 Haemophilus Pasteruella Chapter 35 Bordetella Chapter 36 Francisella Brucella Yu Chun-Keung DVM, PhD Department of Microbiology and Immunology College of Medicine National Cheng Kung University May 5, 2010 Chapter 34 Haemophilus Family Pasteurellaceae Genera Haemophilus Actinobacillus Aggregatibacter Pasteurella Small, G(-), non-spore-forming bacilli Fastidious growth needs Genus Haemophilus “Blood-lover” Growth require hemin (x factor) and nicrotinamide adenine dinucleotide, NAD (v factor) Heated blood (chocolate) agar for isolation Important Haemophilius species H. influenzae (an important pathogen) H. aegyptius (acute, purulent conjunctivitis) H. ducreyi (STD – soft chancre) H. parainfluenzae (rarely pathogenic) Classification H. influenzae (Hi) Serological differentiation - polysaccharide capsular antigens: serotype a to f Biochemical properties - indole production, urease activity, ornithine decarboxylase activity : biotype I to VIII Pathogenesis Non-encapsulated Hi & H. parainfluenzae (non-typeable) Colonize URT in all people 10% of the flora of saliva: H. parainfluenzae Opportunistic pathogens: spread locally and cause acute and chronic otitis, sinusitis, bronchitis, and pneumonia. Pathogenesis - encapsulated Hi type b Uncommon in the URT Common cause of disease in unvaccinated children Adhesins colonization of oropharynx release cell wall components damage and impair ciliary function across epithelial and endothelial cells blood (invasion) Produce IgA1 proteases, facilitate colonization LPS lipid A induces meningeal inflammation Major virulence factor: antiphagocytic polysaccharide capsule – polyribitol phosphate (PRP) : ribose, ribitol, phosphate Phagocytic engulfment of H. influenzae bacterium opsonized by antibodies specific for the capsule and somatic (cell wall) antigen. 2004 Kenneth Todar University of Wisconsin-Madison Department of Bacteriology Natural infection, vaccination, passive transfer of material antibody - antiPRP antibody is protective (enhance phagocytosis and complementmediated bacteriocidal activity) Absence of anti-PRP antibody (complement depletion, splenectomy ) leads to invasion, bacteremia and dissemination Clinical diseases (Hib infection) Meningitis: Hi type b was the most common cause of pediatric meningitis (3 -18 m) results from bacterimic spread from nasopharynx; cannot be differentiated from other causes of bacterial meningitis (S. pneumoniae, N. meningitidis, E. coli). Age-specific incidence of bacterial meningitis caused by Haemophilus influenzae, Neisseria meningitidis and Streptococcus pneumoniae prior to 1985 2004 Kenneth Todar University of WisconsinMadison Department of Bacteriology Clinical diseases (Hib infection) Epiglotitis: 2-4 yrs; swelling of the supraglottic tissue, pharyngitis, fever, rapidly progress to complete obstruction of the airways, life-threatening emergency. Cellulitis: fever, reddish-blue patches on the cheeks or periorbital area. Arthritis: the most common form of arthritis (single large joint) in children <2 yrs. • Before the introduction of conjugated vaccine, Hib was a common pediatric disease in children < 5 yrs. • Polysaccharide vaccine for Hib were not effective for children < 18m (the high risk population). • Hib conjugate vaccine, which can work for infant >2m, was introduced in 1987 which greatly reduced the incidence of disease (>90%). Epidemiology Now Hib infections only occur in nonimmune children or adults with waning immunity, Other serotypes of encapsulated strains and non-encapsulated strains become more common. Hib remains a significant pediatric pathogen worldwide, especially in developing countries. Transmission Person-to-person transmission in nonimmune population Increased disease frequency in households where there is a primary case or an asymptomatic carrier. Primary risk factor for invasive disease = absence of anti-PRP antibody. Close contacts should be given chemoprophylaxis. Diagnosis Clinical diagnosis Sign, Symptom, Syndrome Laboratory diagnosis detection / identification of antigens (whole cell, protein, nucleic acid) detection of immune responses (i.e. antibodies) Signs are those findings that a physician can objectively detect or measure. Symptoms are those problems that a patient notices or feels. Diagnosis Specimens: Oral swab: avoid contamination with oral secretions Direct needle aspiration Sputum from LRT Cerebrospinal fluid and blood (>107 bacteria/ml) Microscopy: both sensitive & specific; G(-) bacilli in CSF in >80% cases before antibiotics treatment Diagnosis Particle agglutination test (for Hib only): Detect PRP antigen, rapid and sensitive (1 ng/ml) Anti-PRP Ab-coated latex particles + specimen, if PRP present, “positive” agglutination Culture: Hib : chocolate agar, colony 1-2 mm. Satellite phenomenon: Hib grows around colonies of Staph. aureus on unheated blood agar. H. aegyptius / H. ducreyi : fastidious Treatment Prompt antimicrobial therapy for systemic Hib infections, otherwise mortality 100% Serious infections: cephalosporins Less severe infections (otitis, sinusitis): ampicillin Antibiotic chemoprophylaxis (rifampin) for high risk group (children < 2ys with patients around) Prevention Hi type b conjugate vaccine Purified capsular PRP + Carrier proteins: Meningococcal outer membrane protein Diphtheria toxoid Tetanus toxoid Three doses of vaccine (the same type) before age of 6 months followed by booster doses. Haemophilus ducreyi Cause of genital ulcers - soft chancre, 軟 性下疳 A sexually transmitted disease; most common in Africa and Asia Indurate and painful ulcer on genitalia with regional lymphadenopathy Differential: syphilis, herpes simplex, lymphogranuloma venereum (caused by Chlamydia trachomatis) Haemophilus aegyptius Koch-weeks bacillus Acute, purulent conjunctivitis Genus Aggregatibacter A. actinomycetemcomitans and A. aphrophilus Mouth flora blood damaged heart valve / artificial valve subacute endocarditis Difficult to diagnosis : develop slowly and the bacteria grow slowly in blood agar (> 5 days) Genus Pasteurella P. multocida and P. canis Primarily animal pathogen. Commensals in oropharynx of health animals. Human infections result from animal contact (bites, scratches, shared food). The most common organism in human wounds inflicted by bites from cats and dogs. Three general forms of disease Localized cellulitis and regional lymphadenopathy after animal bite or scratch. Exacerbation of chronic respiratory tract disease in patients with underlying pulmonary dysfunction. Systemic infection in immunocompromised patients. Lab diagnosis Grows well on blood and chocolate agar Large, buttery colonies with a musty odor Treatment Susceptible to a variety of antibiotics Penicillin, macrolides, tetracycline … Chapter 35 Bordetella Extremely small (0.2 x 1 μm ), G(-), coccobacilli Have simple nutritional requirement Some species (i.e., B. pertussis) are highly susceptible to toxic substances and metabolites in media (need charcoal, starch, blood, or albumin to absorb toxic substances) Important Bordetella species B. pertussis: whooping cough / pertussis (severe cough) B. parapertussis: mild form of pertussis B. bronchiseptica: respiratory disease of animals (pigs and dogs) B. holmesii: uncommon cause of sepsis The four species are closely related, differing only in the expression of virulence genes Pathogenesis • Exposure (aerosol) • Bacterial attachment to ciliated epithelial cells of the respiratory tract by means of adhesins (黏附因子) • Proliferation • Production of toxins • Localized tissue damage and systemic toxicity Colonization of tracheal epithelial cells by Bordetella pertussis 2004 Kenneth Todar University of WisconsinMadison Department of Bacteriology Bacterial adhesins Filamentous hemagglutinin: contain RGD motif: bind (1) sulfated glycoprotein integrins on ciliated respiratory cells; (2) CR3 on macrophages, and trigger phagocytosis without initiating oxidative burst (intracellular survival, escape from Ab) Pertactin : contain RGD motif Pertussis toxin: A classic A-B toxin with a toxic subunit (S1) and binding subunits (S2 to S5); S2 binds lactosylceramide on ciliated respiratory cells, S3 binds phagocytic cells Fimbria : mediate binding in vitro; in vivo function unknown Toxins S1 subunit of pertussis toxin Adenylate cyclase toxin / hemolysin Dermonecrotic toxin Tracheal cytotoxin LPS S1 subunit of pertussis toxin S2-S5 binding subunit S1 toxic subunit Adenosine diphosphateribosylating activity for G protein, which regulates adenylate cyclase activity (convert ATP to cAMP). Increase respiratory secretion and mucus production. Tracheal cytotoxin: (1) target ciliated epithelial cell; ciliostasis, extrusion of ciliated cells, impair regeneration of damaged cells by interfering DNA synthesis (disrupt clearance mechanism, lead to cough); (2) IL-1 production (lead to fever) A tracheal organ culture 72 h after infection with B. pertussis. Large arrow: Bordetella Small arrow: cilia Extruded epithelial cell with attached bacteria Denuded epithelium Normal ciliated epithelial cell Toxins Adenylate cyclase toxin / hemolysin: (1) activated by calmodulin and converse ATP to cAMP, increase respiratory secretion; (2) inhibit leukocyte functions Dermonecrotic toxin: vasoconstriction and tissue destruction LPS: unknown (activate complement and stimulate cytokine release) Clinical disease Infect ciliated epithelial cells of the airways, produce disease locally, no invasion. Catarrhal phase : resemble common cold, sneezing, serous rhinorrhea, malaise, low-grade fever, 1-2 wk, infectious (disease not recognized with high number of bacteria produced) Paroxysmal phase : a series of repetitive coughs followed by inspiratory whoop, vomiting, and exhaustion, 40-50 paroxysms daily, lymphoctyosis, 2-4 wk. Convalescent phase : paroxysms diminish with secondary complications, lasts for above 3 wk. Clinical disease Classic presentation may not be seen in patients with partial immunity. Only chronic persistent cough without whooping or vomiting Differential diagnosis Mycoplasma pneumoniae Chlamydophilia pneumoniae Legionella pneumophila Epidemiology Pertussis was considered a pediatric disease (< 1 year) Incidence (morbidity and mortality) has been reduced considerably after the introduction of vaccine in 1949. Still endemic worldwide with a dramatic increase in recent year in US Majority of infections are found in adolescents and adults (reason not known). 2009.4.23 Lab diagnosis – specimen collection and transport Extremely sensitive to drying, do not survive outside the host or traditional transport medium. Inoculate (nasopharyngeal aspirate) to freshly prepared medium or transport medium at bedside. Use synthetic fiber swabs not cotton swabs (fatty acid are toxic to Bp). Lab diagnosis - microscopy Fluoresceinlabeled rabbit anti-Bp Ab Aspirated specimen Direct Fluorescein-labeled anti-rabbit Ig Ab Rabbit anti-Bp Ab Indirect Direct or indirect fluorescent antibody tests for antigen detection Aspirated specimen microscopic slide airdried heat fixed fluorescent Ab Sensitivity 50% .Nucleic acid amplification Polymerase chain reaction sensitivity 80-100% No FDA approved test, inhouse assay Serology No FDA approved test ELISA for antibodies against filamentous hemagglutinin or pertussis toxin Lab diagnosis - culture Regan-Lowe charcoal medium (horse blood, glycerol, peptones). 35°C, humidified, 7 days, 50% sensitivity, affected by Patient factors (stage of illness, use of antibiotics) Quality of specimen Transport conditions Culture methods Treatment Primarily supportive. Recovery depends on regeneration of ciliated epithelial cells. Antibiotics (erythromycin) are effective and can reduce duration of clinical course. However, the illness is usually unrecognized during catarrhal phase (the peak of contagiousness) Pertussis is highly contagious; prophylaxis for family members of a symptomatic patient. Vaccination DTP vaccine (diphtheria + toxoid of tetanus + inactivated whole cell of Bp), 80-85% effective. DTP vaccine has not been widely accepted because of vaccine-related complications. DTaP (acellular vaccine) : D + T + inactivated pertussis toxin, filamentous hemagglutinin, and pertactin or fimbriae. Pediatic DTaP vaccination: 2, 4, 6, 15-18 m, and 4-6 yrs; Adult DTaP: 11-12 yrs and 19-65 yrs, both high level of protection Chapter 36 Francisella and Brucella Zoonotic pathogens and potential agents of bioterrorism Very small G(-) coccobacilli, 0.5 1.5 m, Fastidious, slow growth on culture (>1 week) Taxonomically unrelated α-Proteobacteria Brucella Rickettsia Ehrlichia γ-Proteobacteria Francisella Legionella Pasteruella Pseudomonas Genus Francisella Francisella tularensis (Tularemia) F. tularensis subsp. tularensis (type A) F. tularensis subsp. holarctica (type B) F. tularensis subsp. Mediasiatica (rare as pathogen) F. tularensis subsp. Novicida (rare as pathogen) Francisella philomiragia (uncommon opportunistic pathogen) Pathogenesis Pathogenic strains possess antiphagocytic capsule; protect bacteria from complement-mediated killing Intracellular parasite Can survive for prolonged periods in macrophages; inhibit phagosomelysosome fusion. IFN-γ- and TNF-α-mediated activation of macrophage is essential for controlling bacterial replication and killing in early stage. Specific T cell-mediated activation of macrophage is essential for controlling bacterial replication and killing in late stage. Epidemiology F. tularensis subsp. tularensis Natural reservoirs and vectors: >200 species of mammals, birds, blood-sucking arthropods Type A: North America: lagomorphs (rabbits, hares), cats, biting arthropod Type B: Northern hemisphere: rodents, cats Hunters, lab personnel and those exposed to ticks are high risk for infection in endemic areas Infections occur in summer and winter; warm winter + wet summer (increase in tick population) Actual numbers of infections > reported cases Clinical disease - Tularemia (Rabbit fever / Tick fever) Clinical symptoms and prognosis determined by route of infection Ulcer Cutaneous tularemia infection microbes.historique.net Ulceroglandular form: cutaneous ulcer + swollen LN, most common Oculoglandular form: painful conjunctivitis + swollen cervical LN. Typhoidal form: sepsis Pneumonic form: pulmonary symptoms Gastrointestinal form: Lab diagnosis Specimen collection: highly contagious: able to penetrate through unbroken skin and mucous membrane + aerosols. extremely hazardous for physician and lab workers; wear gloves and perform work in biohazard hood Microscopy: Grain stain – not practical; direct staining with fluorescent antibody, more sensitive and specific Culture: not grow in common medium without cysteine (eg. blood agar); use chocolate agar or buffered charcoal yeast extract (BCYE) agar, take a week or longer Serology: a 4-fold increase in Ab titer during illness or a single titer of 1:160; antibody persist for many years (past or current infection?); cross-reactivity between Brucella and Francisella T/P/C Penicillin and cephalosporin are ineffective (produce β-lactamase) Streptomycin and gentamicin are effective (high toxicity) Prompt treatment < 1% mortality rate Wear protective clothes and use insect repellents, avoid reservoirs and vectors Prophylactic antibiotics for high risk groups Live-attenuated vaccine : partly protective Genus Brucella Six species with four species associated with human diseases B. melitensis : goat and sheep (natural host) B. suis : swine, reindeer, caribou B. abortus : cattle, bison B. canis : dog, fox, coyotes Pathogenesis No exotoxin, endotoxin low toxicity Smooth colonies associated with virulence Granuloma Accumulation of activated macrophages Obligate intracellular parasites Infect monocytes/macrophages, inhibit phagolysosome fusion. Spread to spleen, liver, lymph node, bone marrow, kidneys (bacteria secrete proteins that induce granuloma) Epidemiology Worldwide distribution Animal reservoirs; natural hosts develop mild or asymptomatic disease. Sterility, abortion, and asymptomatic carriage. Animal tissues (breast, uterus, epididymis, placenta) contain erythritol (紅鮮醇) which is required for the growth of the organism. Milk, urine and birth products contain high number of bacteria. Epidemiology Human infections Direct contact: a lab or occupational exposure Ingestion: consume contaminated food products Inhalation Sources of Brucella infection. G.G. Alton & J.R.L. Forsyth Clinical disease (Brucellosis, Bang’s disease, undulant fever, Malta fever) Disease spectrum depends on the infecting organism B. melitensis : severe disease B. suis : severe and chronic B. abortus : mild B. canis : mild Clinical disease Acute disease: incubation period 1-3 wks, fever rises in afternoon, fall during night with drenching sweat (undulant fever), weakness, malaise, chill, weight loss, nonproductive cough, aches, pain. Advanced disease: involve many tissues, granulomas and abscesses. 70% GI symptoms, 20-60% bone lesions, 25% respiratory tract symptoms Chronic infection occur in inadequately treated patients. Lab diagnosis Difficult Multiple sampling (blood, bone marrow, infected tissues) Microscopy: insensitive (small size and intracellular location) Culture: blood agar, > 3 days to 2 wks, sensitive and specific Lab diagnosis - serology A significant increase in Ab titer = evidence of current disease; antibodies detected in all patients (IgM, then IgA and IgG) and persist for months and years. 5-10% of population in endemic area have high Ab titer (>1:160) Serologic test: use to confirm clinical diagnosis, not as a basis of diagnosis. Serum agglutination test (SAT): a fourfold increase in titer or a single titer >1:160. B. abortus cross-react with B. melitensis and B. suis, but not with B. canis. T/P/C Tetracycline (doxycycline): bacteriostatic drugs, relapse is common (due to inadequate therapy, not antibiotic resistance); use doxycycline + rifampin for > 6 weeks. No vaccine for humans Control of disease in livestock Identification (serologic testing) Elimination of infected herds Vaccination Avoidance of unpasturized dairy products Observance of safety procedures in clinical lab