Miscellaneous Bacteria
advertisement
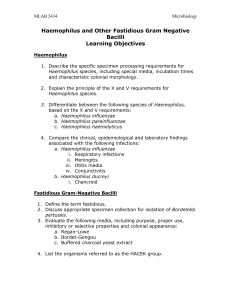
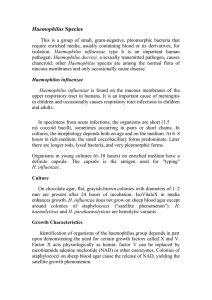
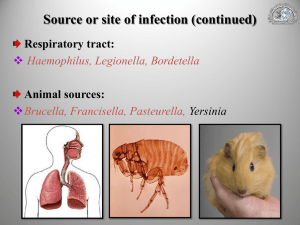
Fe A. Bartolome, MD, DPASMAP Department of Microbiology & Parasitology Our Lady of Fatima University HAEMOPHILUS • Family Pasteurellaceae • Small, gram negative, pleomorphic • Require enriched media containing blood or its derivatives • Facultative anaerobes • Obligate parasites Haemophilus influenzae • Found on mucus membrane of URT in humans (noncapsular form) encapsulated species uncommon members of normal flora • Short, coccoid bacilli in pairs or chains Haemophilus influenzae Classification: 1. Serotype – based on capsular antigen 2. Biotype – based on biochemical properties a. indole production b. urease activity c. ornithine decarboxylase activity 3. Biogroup – useful for clinical purposes Haemophilus influenzae Culture: • Chocolate agar – flat, grayish brown colonies after 24 hrs incubation • Does not grow on sheep blood agar except around colonies of Staphylococci “satellite phenomenon” Haemophilus influenzae Growth Characteristics: • Requires X factor (hemin) and V factor (NAD) • Ferments carbohydrates poorly and irregularly Haemophilus influenzae Characteristics & Growth Requirements: Species X factor V factor Hemolysis H. influenzae H. parainfluenzae H. ducreyi H. haemolyticus H. parahaemolyticus H. aphrophilus + + + - + + + + - + + - Haemophilus influenzae Virulence Factors: Capsule • Antiphagocytic; impair ciliary function • Main virulence factor • With capsular polysaccharides (a to f) Type b – polyribose-ribitol phosphate (PRP) Haemophilus influenzae Virulence Factors: Somatic antigen • Outer membrane proteins lipooligosaccharides (endotoxin) IgA1 proteases Haemophilus influenzae Clinical Features: H. influenzae type b • Most common serotype causing systemic disease 1. Meningitis 2. Pneumonia & empyemia 3. Epiglottitis 4. Cellulitis 5. Septic arthritis Haemophilus influenzae Clinical Features: Non-typeable (non-encapsulated) H. influenzae • opportunistic 1. Chronic bronchitis 2. Otitis media 3. Sinusitis 4. Conjunctivitis Haemophilus influenzae Clinical Features: Meningitis • 20 to bacteremic spread from nasopharynx • Peak incidence: 3 – 18 mos. Old Epiglottitis • Cellulitis & swelling of supraglottic tissues • Pharyngitis, fever & dyspnea complete airway obstruction death Haemophilus influenzae Clinical Features: Cellulitis • Reddish blue patches on cheeks or periorbital areas Haemophilus influenzae Clinical Features: Arthritis • Infection of a single large joint • Children < 2 y/o or immunocompromised patients or those with previously damaged joints Conjunctivitis • Epidemic and endemic • H. influenzae biogroup aegypticus Haemophilus influenzae Clinical Features: Sepsis with gangrene Haemophilus influenzae Prevention: 1. Chemoprophylaxis with Rifampin for non-immune children < 4 y/o who are close contacts 2. Hib conjugate vaccine • > 2 mos. Old Hib conjugated with C. diphtheriae toxin protein or N. meningitidis outer membrane complex • > 15 mos. Old Hib conjugated with diphtheria toxoid Haemophilus aegypticus • H. influenzae biotype III • Koch-Weeks bacillus • Resembles H. influenzae closely • Diseases: 1. Conjunctivitis – highly communicable 2. Brazilian purpuric fever – fever, purpura, shock and death Haemophilus ducreyi • Causes chancroid (soft chancre) • Ragged ulcer on genitalia with marked swelling and tenderness • Lymph nodes enlarged and painful • Organism grows best on chocolate agar incubated in 10% CO2 • No permanent immunity Haemophilus ducreyi Bordetella pertussis • Small, coccobacillary, encapsulated, gram (-) • With bipolar metachromatic granules (toluidine blue stain) • Non-motile; strict aerobe • Forms acid from glucose and lactose • Requires enriched media Bordet-Gengou medium (potato-blood-glycerol agar) Contains Pen G 0.5 ug/mL • Virulence genes – bvgA and bvgS Bordetella pertussis Gram stain Culture on chocolate agar Bordetella pertussis Virulence Factors: 1. Filamentous hemagglutinin • Protein on pili; adhesion to ciliated epithelial cells 2. Pertussis toxin a. promote lymphocytosis via inhibition of signal transduction by chemokine receptors lymphocytes do not enter lymphoid tissues b. promote sensitization to histamine c. enhance insulin secretion d. stimulate adenylate cyclase via ADP-ribosylation Bordetella pertussis Virulence Factors: 3. Adenylyl cyclase toxin – inhibit phagocytosis 4. Tracheal cytotoxin • Fragment of bacterial peptidoglycan • Induce nitric oxide destroy ciliated epithelium 5. Dermonecrotic toxin 6. Hemolysin Bordetella pertussis Pathogenesis: • Adheres to and multiplies rapidly on epithelial surface of trachea and bronchi interfere with ciliary action • No invasion of blood Bordetella pertussis Clinical: • MOT: airborne droplets • Source of infection: patients in early catarrhal stage • Disease: Pertussis or Whooping Cough acute tracheobronchitis • Incubation period: approx. 2 weeks Bordetella pertussis Clinical: Stages of Disease 1. Catarrhal • Mild coughing and sneezing • Highly infectious but not very ill 2. Paroxysmal (1-4 weeks) • Series of hacking coughs, accompanied by copious amts. of mucus, ending with inspiratory “whoop” exhaustion, vomiting, cyanosis and convulsions • High wbc count (16,000-30,000/uL) with absolute lymphocytosis 3. Convalescence - slow Bordetella pertussis Laboratory Diagnosis: Specimen: saline nasal wash (preferred) or nasopharyngeal swab 1. Direct fluorescence antibody test – 50% sensitivity 2. Culture of saline nasal wash fluid 3. PCR – most sensitive 4. Serology – (+) only on third week of illness of little diagnostic value Bordetella pertussis • First defense is antibody that prevents attachment • Recovery from disease or immunization is followed by immunity • Second infection may occur but is mild • Re-infection occurring years later in adults may be severe • Vaccine-induced immunity not completely protective Bordetella pertussis Prevention: 1. Chemoprophylaxis – Erythromycin for exposed, unimmunized individuals OR exposed, immunized children < 4 years old 2. Vaccine – two vaccines available: a. acellular vaccine – contains 5 purified antigens main immunogen is inactivated pertussis toxin; first vaccine to contain a genetically inactivated toxoid ADP-ribosylating activity removed b. DPT x 3 doses BRUCELLA • Zoonotic obligate parasite of animals & humans • Intracellular organism • Gram negative coccobacilli • Aerobic; non-motile; nonspore-forming • Catalase (+); oxidase (+) • Produces H2S • Culture: trypticase soy agar OR blood culture media; B. abortus requires 5-10% CO2 for growth BRUCELLA • Route of infection in humans: 1. Intestinal tract – ingestion of infected milk & contaminated dairy products (cheese from unpasteurized goat’s milk) 2. Mucous membranes – droplets 3. Skin – contact with infected tissues of animals • Pathogenesis: endotoxin – O antigen polysaccharide BRUCELLA Species Animal Pathology B. melitensis Goats Acute & severe infection B. suis Swine Chronic w/ suppurative lesions; caseating granulomas B. abortus Cattle Mild disease w/o suppuration; non- caseating granulomas of the RES (LN, liver, spleen, BM) B. canis Dogs Mild disease BRUCELLA Clinical: Brucellosis (Undulant or Malta Fever) 1. Acute • Malaise, fever, weakness, aches & sweats • Fever rises in the afternoon fall during the night with drenching sweats • (+) lymphadenopathy w/ palpable spleen; + hepatitis with jaundice 2. Chronic • With psychoneurotic symptoms • Weakness, aches & pains, low grade fever BRUCELLA Diagnosis: 1. Culture • BM & blood – commonly used specimen • Brucella agar, trypticase soy medium, brain heart infusion medium, chocolate agar 2. Serology – inc. IgM during 1st week of illness; peak at 3 months Francisella tularensis • Small, gram (-) pleomorphic rod • Widely found in animal reservoirs (rabbits, deer, rodents) • Humans are accidental “dead-end” hosts • Two biotypes: 1. Jellison type A – more virulent ; US 2. Jellison type B – less virulent ; Europe • Culture: glucose cysteine blood agar OR glucose blood agar Francisella tularensis Gram stain F. tularensis colonies on agar plate Francisella tularensis Mode of transmission: 1. Contact with animal tissue 2. Bite of vector (Dermacentor tick) 3. Ingestion of infected meat 4. Inhalation Symptoms caused by endotoxin Francisella tularensis Clinical: 1. Ulceroglandular – 75%; ulceration at site of entry with swollen & painful LN 2. Glandular 3. Oculoglandular 4. Typhoidal 5. GI & pulmonary Disease confers lifelong immunity Francisella tularensis Cutaneous tularemia Francisella tularensis Diagnosis: culture not done due to high risk to lab workers 1. Agglutination test – most frequently used 2. Fluorescent antibody staining of infected tissue Treatment: Streptomycin (DOC) Prevention: live, attenuated vaccine – partial immunity; not available commercially YERSINIA • Short, pleiomorphic gram (-) rods with bipolar staining • Catalase and oxidase (+) • Microaerophilic or facultative anaerobe • All with LPS that have endotoxic activity Yersinia pestis • Non-motile, facultative anaerobe • Growth more rapid in media containing blood or tissue fluids at 300C gray and viscous colonies Yersinia pestis Virulence Factors: 1. LPS – endotoxin 2. Envelope – with protein (fraction I) antiphagocytic 3. Coagulase 4. V-W antigens (virulent, wild type) – essential for virulence 5. Pesticin - bacteriocin Yersinia pestis Pathogenesis: 1. Bite of vector (Xenopsylla cheopis) organism phagocytosed by PMNs & monocytes multiply in monocytes lymphatics (+) intense hemorrhagic inflammation in enlarged LN bloodstream hemorrhagic & necrotic lesions in all organs 2. Inhalation of infective droplets from coughing patients primary pneumonic plague with hemorrhagic consolidation, sepsis and death Yersinia pestis Clinical: Plague • I.P.: 2 – 7 days • High fever & painful lymphadenopathy (buboes) • Vomiting & diarrhea may develop with early sepsis • Later DIC hypotension, altered mental status, renal and cardiac failure • Terminal: signs of pneumonia & meningitis Yersinia pestis Bubo on neck Septicemic plague Yersinia pestis Diagnosis: 1. Smear – Giemsa stain or Wayson’s stain (+ bipolar appearance) 2. Culture – blood agar or MacConkey’s agar plates; infusion broth; all cultures highly infectious 3. Serology - examination of acute and convalescent sera for antibody levels Treatment: Streptomycin (DOC) Pasteurella multocida • Primarily animal pathogens • Non-motile gram (-) coccobacilli with bipolar appearance on stained smears • Occurs worldwide in respiratory tract and GIT of many domestic and wild animals • Most common organism in human wounds inflicted by bites from cats and dogs • Virulence factors include capsule and endotoxin Pasteurella multocida Clinical: • Rapidly spreading cellulitis at site of animal bite • Incubation period < 24 hours • May present as bacteremia or chronic respiratory infection • Complication: osteomyelitis (cat bites) Treatment: Penicillin G (DOC) Pasteurella multocida Culture P. multocida infection Bacteremic P. multocida cellulitis