Acute Abdomen
advertisement

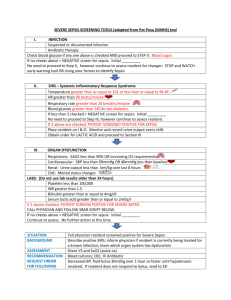
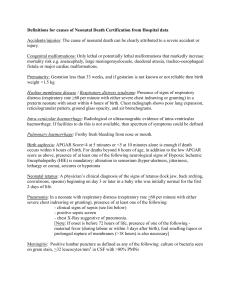
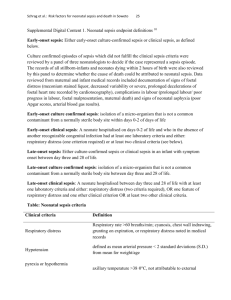
Neonatal Sepsis NICU Night Team Curriculum Sepsis: Objectives • • • • • Define Sepsis Review common pathogens causing sepsis in a neonate Review clinical findings Review the initial work up of an infant suspected of having sepsis Review initial management of neonatal sepsis While on call in the NICU… • The nurse pages: A 6 hr-old 36 wk female has developed apenic and bradycaridic episodes • Infant was born to G1P1 mother via NSVD who developed a temperature of 39.1 shortly before the fetus was delivered. Maternal serologies were negative except for a GBS positive urine culture at 20 weeks GA. Mom received 1 dose of antibiotics secondary to a precipitous delivery. Pregnancy was otherwise unremarkable. • Infant has been in NICU x 6 hours receiving Ampicillin and Gentamicin Physical exam • T:36.5C, P:170, RR:62, MAP:33, SpO2: 92% on 1LNC • Gen/Head: AFOSF, atraumatic • CV: Tachycardic rate with observed episodes of bradycardia during exam with lowest observed heart rate of 85, NL S1/S2, No murmur. Cap refill ~3 sec • Pulm: Tachypnic rate, subcostal retractions observed. No crackles, no rales/rhonchi. • Abd: Soft, non-tender, non-distended. • Skin: No rash, petechiae or purpura. Neonatal Sepsis • Definition: – A clinical syndrome in an infant 28 days of life or less, manifested by systemic signs of infection and/or isolation of a bacterial pathogen from the blood stream (Edwards, 2004) • Further Classification: – Early-onset: Onset of symptoms in first 6 days of life – Late-onset: Onset of symptoms after first week of life Pathogenesis • Early-onset sepsis: – Vertical transmission • Contaminated amniotic fluid • Vaginal bacteria – Increased risk with maternal chorioaminitis • Late-onset sepsis: – Vertical transmission causing neonatal colonization that later results in infection – Horizontal Transmission • Environmental exposures • Introduction from instrumentation – Increased risk with any interruption of fetal immune system Clinical Findings • Subtle changes in baseline behavior and feeding patterns • Fetal distress during delivery • Most common findings: – – – – – – – Hyperthermia Respiratory distress Poor feeding Vomiting Jaundice Hepatomegaly Lethargy • Less frequently seen: – – – – – Cyanosis Hypothermia Irritability Apnea Abdominal Distension Back to the patient… You are at the bedside and the patient is continuing to have bradycardic episodes throughout the exam • What are your first steps in evaluation? • How would you treat this patient? Evaluation • Culture all body fluids – Blood • Positive blood culture is the only method of truly diagnosis neonatal sepsis – CSF – Urine • Not necessary in infants <6 days as UTIs are rarely the source of sepsis – Any other sites of infection (pustules, purulent eye drainage) • CBC – Increased suspicion with: • WBC count <5000/microL • Absolute neutropenia • Elevation of immature white blood cells when compared to PMNs (I:T ratio) (Newman, 2010) • CRP – Value of > 1.0 mg/dL has a 90% sensitivity of detecting sepsis (Pourcyrous, 2003) but is not specific and increases in response to many other factors (maternal fever, hypoxia, IVH) – Most value when trend is followed over time • Chest x-ray with signs of respiratory distress Management Antibiotic Therapy – Empiric coverage for common pathogens • Early-onset – Ampicillin and Gentamicin • Late-onset – Ampicillin and Gentamicin – Vancomycin subsituted for Ampicillin for those with possible CONS or MRSA infection – Clindamycin for those with suspected anaerobic infections – Narrow coverage after organism is identified – Duration depends fluid from which organism was isolated Supportive Care – Fluid resuscitation • Crystalloid • Colloid – Pressor support in those who do not respond to fluid – Electrolyte replacement – Ventillatory support when necessary References • • • Edwards MS, Baker CJ. Sepsis in the Newborn. Krugman's Infectious Diseases of Children, 11th, Gershon AA, Hotez PJ, Katz SL (Eds), Mosby, Philadelphia 2004. p.545. Newman TB, Puopolo KM, Wi S, Draper D, Escobar GJ. Interpreting complete blood counts soon after birth in newborns at risk for sepsis. Pediatrics. 2010;126(5):903. Pourcyrous M, Bada HS, Korones SB, Baselski V, Wong SP. Significance of serial C-reactive protein responses in neonatal infection and other disorders. Pediatrics. 1993;92(3):431.